26 April 2022: Original Paper
Postoperative Health Status and Quality of Life After Pure Laparoscopic Donor Hepatectomy for Living Donor Liver Transplantation
Chan Woo Cho1CE, Gyu-Seong Choi2AB*, Jong Man Kim2B, Jinsoo Rhu2B, Choon Hyuck David Kwon3AF, Jae-Won Joh2ABDOI: 10.12659/AOT.935611
Ann Transplant 2022; 27:e935611
Abstract
BACKGROUND: Laparoscopic donor hepatectomy (LDH) for living donor liver transplantation has been performed in several specialized institutes. Surgical outcomes of LDH have shown comparable results to open donor hepatectomy (ODH), but the quality of life (QOL) after LDH is not known. This prospective questionnaire-based study was performed to assess health status and QOL of live liver donors before and after donor hepatectomy (DH).
MATERIAL AND METHODS: From May 2017 to February 2020, questionnaire items such as the Enhanced Recovery after Surgery mobility scale (EMS), Body Image Questionnaire, and EQ-5D-3L were examined up to 1 year after DH to respectively evaluate postoperative recovery, body image satisfaction, and health status.
RESULTS: During the study period, 45 laparoscopic DH (LDH) donors and 2 open DH (ODH) donors were finally fully evaluated. The LDH group had a significantly higher mean EMS than ODH on postoperative day (POD) 5, and 7 (P=0.011, and P=0.004, respectively). Body image scores of the LDH group were significantly higher than that of the ODH group at 1 month after DH (17.8 vs 15.0, P=0.017). There were 45 LDH donors who recovered to preoperative values at 6 months and 1 month after DH, with no statistically significant difference in EQ-5D-3L index value and visual analogue scale (P=0.059 and P=0.217, respectively).
CONCLUSIONS: Within 1 month after DH, LDH donors showed faster mobility recovery and body image satisfaction to the level of preoperative status than ODH. LDH donors recovered to preoperative health status within 6 months, in accordance with previous studies of ODH donors.
Keywords: Liver Transplantation, Living Donors, Quality of Life, Hepatectomy, Humans, Laparoscopy, Liver, Prospective Studies, Tissue and Organ Harvesting
Background
Living donor liver transplantation (LDLT) is the established treatment option for patients with end-stage liver disease, especially in Asia, where deceased donor livers are scarce. Liver donation for LDLT requires healthy donors to undergo major surgery, and donor safety is one of the most important issues in performing LDLT. A worldwide survey reported that the operative mortality rate of the live liver donor was 0.2% (23/11 553), with the majority of deaths occurring within 60 days [1]. According to a recent nationwide study of 10 116 live liver donors in Korea, 10-year cumulative mortality of live liver donors was 0.9% and was significantly lower than that of the general population [2]. Along with donor safety, recovery to pre-donation quality of life (QOL) is also a significant consideration in LDLT. In a systematic review including 19 studies, most live liver donors returned to their baseline QOL within 6 months after LDLT [3].
Over the past 2 decades, laparoscopic liver resection (LLR) has been widely adopted as the accumulation of surgeon experience and the development of surgical skills and equipment has increased [4]. In many studies comparing LLR with open liver resection (OLR), LLR has been shown to reduce postoperative complications such as surgical site infection and ascites, to shorten hospital stay, and to return to normal activity earlier than in OLR [5].
The laparoscopic approach to donor surgery is ideal for liver donation in healthy individuals. While Cherqui et al first reported laparoscopic donor left lateral sectionectomy for a paediatric recipient in 2002 [6], pure laparoscopic donor hepatectomy (PLDH) for adult LDLT is still limited, and it is still considered to be in the developmental phase (IIa) according to the Balliol classification scheme of the IDEAL model [7,8]. There have been successful studies of PLDH at several experienced centers, but most are reports regarding postoperative surgical outcomes of laparoscopic donor hepatectomy (LDH) compared with those of the open donor hepatectomy (ODH) patients [9–11]. Therefore, we performed this prospective questionnaire-based study to compare postoperative health status, including postoperative recovery, body image satisfaction, and QOL between the ODH and LDH groups after DH.
Material and Methods
PATIENTS AND STUDY DESIGN:
This study was designed as a single-center prospective registry of donors who could not be randomized due to patient or surgeon preference. The Institutional Review Boards of our center (number 2017-03-004) approved this study. From May 2017 to February 2020, 70 donors were included in this study after assessment for eligibility for liver donation. After intensive discussion between the surgeon and the donor, the operation type (ODH or LDH) was selected according to donor preference and therefore could not be randomized. At the beginning of the study, 5 and 65 donors selected ODH and LDH, respectively. Eight patients who refused the survey and 15 patients who did not visit outpatient clinics were excluded from the study. Finally, the number of subjects in the ODH and LDH groups were 2 and 45, respectively (Figure 1). The following clinical data were collected from registered patients: demographic factors including age, sex, and body mass index (BMI), surgical factors including donor hepatectomy type, operation time, blood loss, transfusion, and Pringle manoeuvre time, and postoperative factors including hospital stay and complications.
SURGICAL PROCEDURE:
The intraoperative surgical technique was standardized. Operations were performed by 2 surgeons (GS Choi or JM Kim). In ODH, patients were in the supine position and the operations were carried out using an upper midline incision. In LDH, the patients were in the French position. All LDHs were performed using the pure laparoscopic approach using 5 trocars and a 3D flexible scope. Detailed surgical procedures are described in a previous study [10].
EVALUATION TOOLS FOR RECOVERY OUTCOMES MEASUREMENT:
As shown in Figure 1, a survey for health status assessment and QOL was conducted on the day before the operation, during hospitalization, on the discharge date, and 1 month, 6 months, and 12 months after DH, based on the following evaluation tools:
THE ENHANCED RECOVERY AFTER SURGERY (ERAS) MOBILITY SCALE:
The ERAS Mobility Scale (EMS) was used to evaluate postoperative recovery of mobility. EMS uses 10 action items to compare mobility level before and after DH during hospitalization. Patients were considered independently mobile when they reached their preoperative EMS level or scored positive points on 8 out of 10 items [12].
THE BODY IMAGE QUESTIONNAIRE (BIQ):
The BIQ was utilized to assess body image and cosmesis based on 8 questions. Body image was defined based on multidimensional structures that indicate how patients think, feel, and act based on their physical characteristics, including incisional scars [13]. Cosmesis is defined as the level of a clear satisfaction with incisional scars [14]. Body image assessment was performed preoperatively at the time of consent, at discharge, and at 1, 6, and 12 months after surgery.
:
The EQ-5D is a standardized, generic, health-related QOL questionnaire developed by the EuroQol Group [15]. This study used the EQ-5D-3L version to evaluate the health status of 45 liver donors who underwent LDH. The EQ-5D-3L assesses 5 dimensions including mobility (M), self-care (SC), usual activity (UA), pain/discomfort (PD), and anxiety/depression (AD), with 3 levels (Level 1: no problems, Level 2: some problems, Level: extreme problems) and a rating on the EQ visual analogue scale (EQ-VAS; 0–100). The descriptive system element of the EQ-5D questionnaire produces a 5-digit health state profile (eg, 32332; see Table 1). EQ-5D health state was subsequently converted into a single summary number with the term of “index value” according to the preferences of the general population of South Korea (Table 1) [16]. Assessment of donor health status was performed at the time of consent (pre-operation), discharge, and at 1, 6, and 12 months after surgery.
STATISTICAL ANALYSIS:
Continuous data are presented as the mean±standard deviation [SD]. Categorical data are described in numbers and percentages. Statistical analysis was conducted using an independent-samples
Results
PATIENT DEMOGRAPHICS AND SURGICAL OUTCOMES:
Table 2 shows the demographic, surgical, and postoperative characteristics of 47 donors who underwent DH. Of the 70 liver donors registered in this prospective study, 47 patients (2 in the ODH group and 45 in the LDH group) completed the questionnaire up to 1 year after surgery. The median age of the included patients was 27 years, ranging from 18 to 55 years. A total of 31 patients (68.9%) were male, and the median body mass index was 23.4, ranging from 16.9 to 33.4. A total of 45 patients (95.7%) underwent right hemihepatectomy. The LDH group showed significantly longer operation time than the ODH group (255.3±44.1 vs 189.5±5.0, P=0.042). There was no transfusion or open conversion. All but 2 donors in the LDH group were discharged on postoperative day (POD) 6 to 16 without specific complications. Two patients had biliary stricture and leakage, respectively, and were treated by endoscopic retrograde biliary drainage.
POSTOPERATIVE RECOVERY OF MOBILITY:
Figure 2 shows EMS scored during hospitalization in ODH and LDH patients. Two patients in the OLH group were discharged on POD 8 and POD 10, respectively, with neither of the 2 achieving the level of being independently mobile (EMS ≥8). On the contrary, patients in the LDH group were considered independently mobile from POD 5 based on the mean EMS of 45 patients. The LDH group had a significantly higher mean EMS than the ODH group on POD 5 and 7 (P=0.011 and P=0.004, respectively).
BODY IMAGE AND COSMESIS:
Body image scores of the LDH group were significantly higher than in the ODH group at 1 month after DH (17.8 vs 15.0, P=0.017; Figure 3). At 1, 6, and 12 months after DH, cosmesis scores tended to be higher in the LDH group than in the ODH group, but the differences were not statistical significance (P=0.056, P=0.895, and P=0.633, respectively).
HEALTH STATUS AND QUALITY OF LIFE:
Table 3 shows the EQ-5D reporting levels in the 45 live liver donors before and after LDH for LDLT. Compared with preoperative health status, 1 (2%), 3 (7%), and 12 (27%) patients reported new problems (level 2 or 3) at 6 months after LDH in SC, UA, and PD dimensions, respectively. No patients reported new problems at 6 months after LDH in the M and AD dimensions. Based on the percent change in reporting problems, time to return to preoperative health status in the M, SC, UA, and AD dimensions were at 6 months, 12 months, 12 months, and discharge after LDH, respectively. However, patients did not recover to the level of preoperative health status in the PD dimension even 12 months later, and 9 patients (20%) reported some problems compared to before surgery in the PD dimension. The 45 patients recovered quickly in the AD, M, SC, UA, and PD dimensions in terms of mean values and percent changes of levels at 6 months after LDH (Figure 4, Table 3). The EQ-5D-3L index value and EQ-5D-3L VAS were not different from preoperative values at 6 months (P=0.059) and 1 month (P=0.217), respectively (Figure 5).
Discussion
In recent decades, LLR has been widely used by hepatobiliary surgeons, and its indication has expanded to donor hepatectomy in experienced centers. Recent studies have shown that LDH for LDLT is safe and feasible in terms of surgical outcomes compared to ODH [17,18]. Therefore, if the safety of the live liver donor is secured, it is desirable to perform laparoscopic surgery on the liver donor for early recovery after donor hepatectomy. In previous studies at our center, it was reported that the LDH group had smaller estimated blood loss, shorter operation time, shorter hospital stay, and similar major complication rate compared the ODH group [10,17,19–21].
Many studies have been conducted on the QOL and long-term outcome of live liver donors who underwent ODH. A systematic literature review concluded that most liver donors recovered to preoperative QOL within 6 months after surgery [3]. In previous studies of long-term outcome of live liver donors, good health-related QOL for up to 20 years and no regret regarding willingness to donate were reported [22–24]. However, since LDH is a relatively recent procedure, there are no reports of postoperative health status for liver donors who underwent the LDH procedure. Furthermore, postoperative recovery, body image satisfaction, and QOL in donors undergoing LDH have not yet been studied compared to donors undergoing ODH.
The original purpose of this study was to compare LDH and ODH and to determine whether the laparoscopic approach has better post-donation QOL than the open approach in DH. However, at the time of enrolment in the study, only 5 out of 70 donors chose open hepatectomy for liver procurement, 3 of whom were excluded from the study due to study refusal (n=1) and follow-up loss (n=2), leaving only 2 ODH patients, which is less representative and required nonparametric statistical methods to compare the ODH and LDH groups. Group randomization could not be performed due to the special ethical considerations of donor surgery. After an in-depth interview with a surgeon, donors chose the method of surgery on their own, and most donors chose the laparoscopic approach. It can be inferred that the majority of donors are aware of the advantages of laparoscopic surgery, such as cosmetic excellence, less pain, and quick recovery. There was no difference in mean hospital stay between the ODH and LDH groups (9.0 and 8.3 days, respectively;
BIQ failed to show that LDH had a positive impact on body image as compared with ODH, except for the first month after surgery. However, since the LDH group tended to score noticeably higher than the ODH group in cosmesis, a statistically significant difference could have been confirmed if the sample size of ODH group was large enough.
The 45 donors of the LDH group showed the fastest recovery in the AD dimension among the EQ-5D-3L dimensions. Six donors already reported level 2 (somewhat anxious and depressed) in the AD dimension before LDH. However, only 2 donors reported level 2 in the AD dimension 1 year after LDH.
It was reported that the death of the recipient after LDLT had a negative psychological effect on the respective live liver donor, including anxiety, depression, and hopelessness [25]. In this study, 3 of 70 recipients died within 1 year after LDLT, and 3 donors who donated to the expired 3 recipients refused to keep participating in the study. Therefore, recovery of the LDH group may have been better than the actual result.
To comprehensively evaluate the health status of donors, the pre- and post-operative health conditions were compared using EQ-VAS and EQ-5D index values developed according to the preferences of the general population of South Korea. There was no statistically significant difference from preoperative health status at 1 and 6 months after surgery in EQ-VAS and EQ-5D index values, respectively, indicating that the 45 donors who underwent LDH recovered to preoperative health status at least within 6 months after surgery. This is comparable to the results of a systematic review including 19 studies regarding the QOL of donors undergoing ODH [3]. However, many of the studies in this systemic review used the SF-36 as a QOL measurement tool [26–30]. The SF-36 is a generic non-preference-based health status measure that assesses health across 8 dimensions using 36 items. The SF-36 can be used to generate a preference-based index via the SF-6D [31]. No SF-6D weight estimation studies have been conducted in South Korea.
The EQ-5D-3L is a generic preference-based measurement tool developed by the EuroQoL Group and is one of the most commonly used QOL assessment tools in clinical research, along with the SF-36. The EQ-5D-3L has the advantage of self-assessment as the main method of investigation and is relatively easier to use than other tools. In South Korea, an index value was developed by estimating the weight of QOL using EQ-5D-3L. For these reasons, the QOL of donors undergoing LDH was measured in this study using EQ-5D-3L rather than SF-36. It turned out that the mapping relationship between the EQ-5D index value and the SF-36 is reliable based on a previous study [32].
Since it was difficult to recruit the ODH group in our single-center prospective study, early recovery of the LDH group to preoperative baseline health status compared to the ODH group could not be demonstrated. Over the past 5 years, the proportion of LDH in total liver donor surgery at our center has been 90%, and since last year our center has conducted all liver donor surgery for LDLT using the pure laparoscopic approach. Given this trend, it is unlikely that our single-center study for comparison of QOL between the LDH and ODH groups will be able to proceed.
Conclusions
In conclusion, donors undergoing LDH showed faster (within 1 month) mobility recovery and return of body image satisfaction to the level of preoperative status than donors undergoing ODH. In the evaluation of QOL using EQ-5D, donors who underwent LDH recovered to preoperative health status within 6 months, in accordance with previous studies of donors with ODH. A multi-center prospective study is needed to compare the LDH and ODH groups.
Figures
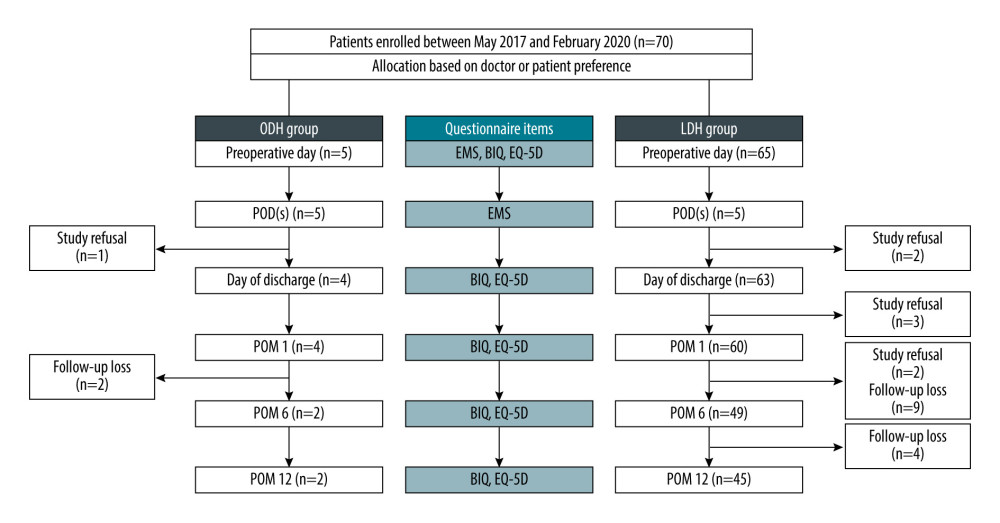 Figure 1. Study flow chart. Figure was created using Microsoft Power Point version 2019. BIQ – Body Image Questionnaire; EMS – ERAS mobility score; LDH – laparoscopic donor hepatectomy; ODH – open donor hepatectomy; POD – postoperative day(s); POM – postoperative month(s).
Figure 1. Study flow chart. Figure was created using Microsoft Power Point version 2019. BIQ – Body Image Questionnaire; EMS – ERAS mobility score; LDH – laparoscopic donor hepatectomy; ODH – open donor hepatectomy; POD – postoperative day(s); POM – postoperative month(s). 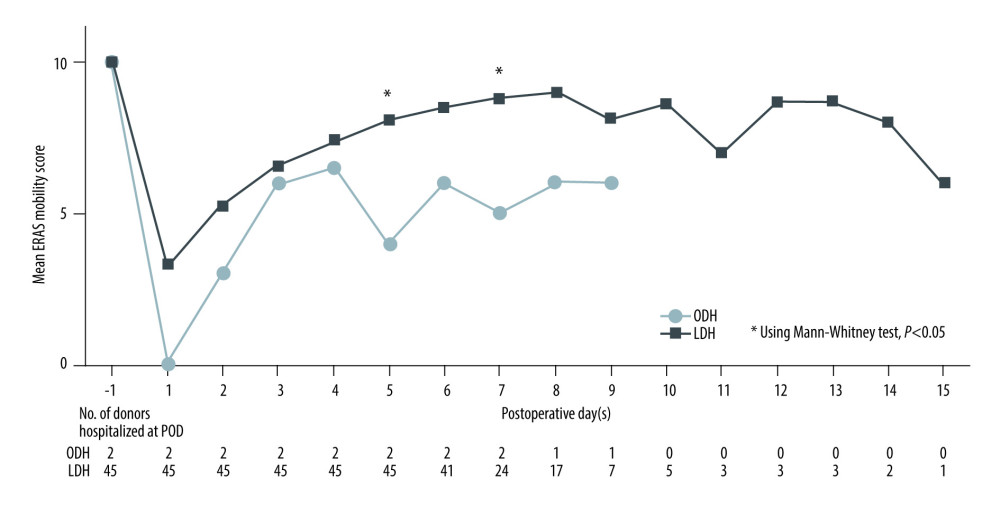 Figure 2. Mean ERAS mobility score between the ODH and LDH groups during hospitalization after DH. Figure was created using Microsoft Power Point version 2019. LDH, laparoscopic donor hepatectomy; ODH, open donor hepatectomy; POD, postoperative day(s).
Figure 2. Mean ERAS mobility score between the ODH and LDH groups during hospitalization after DH. Figure was created using Microsoft Power Point version 2019. LDH, laparoscopic donor hepatectomy; ODH, open donor hepatectomy; POD, postoperative day(s). 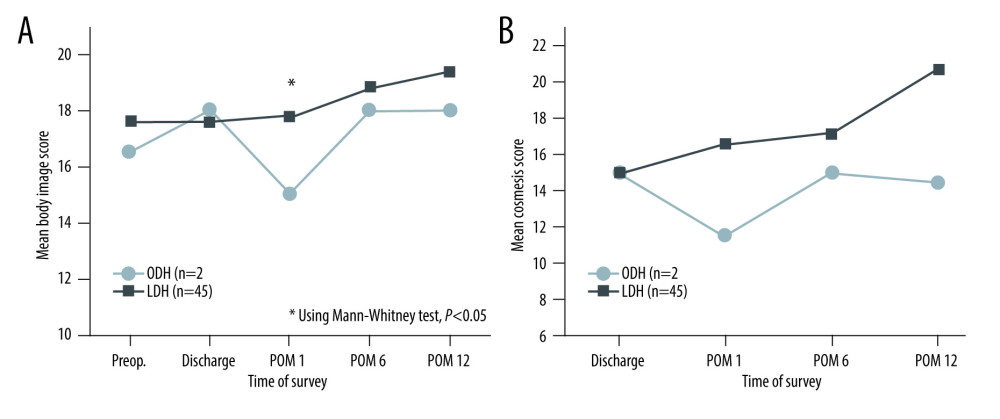 Figure 3. Mean body image score (A) and cosmesis score (B) between the ODH and LDH groups. Figure was created using Microsoft Power Point version 2019. LDH – laparoscopic donor hepatectomy; ODH – open donor hepatectomy; POM – postoperative month(s).
Figure 3. Mean body image score (A) and cosmesis score (B) between the ODH and LDH groups. Figure was created using Microsoft Power Point version 2019. LDH – laparoscopic donor hepatectomy; ODH – open donor hepatectomy; POM – postoperative month(s). 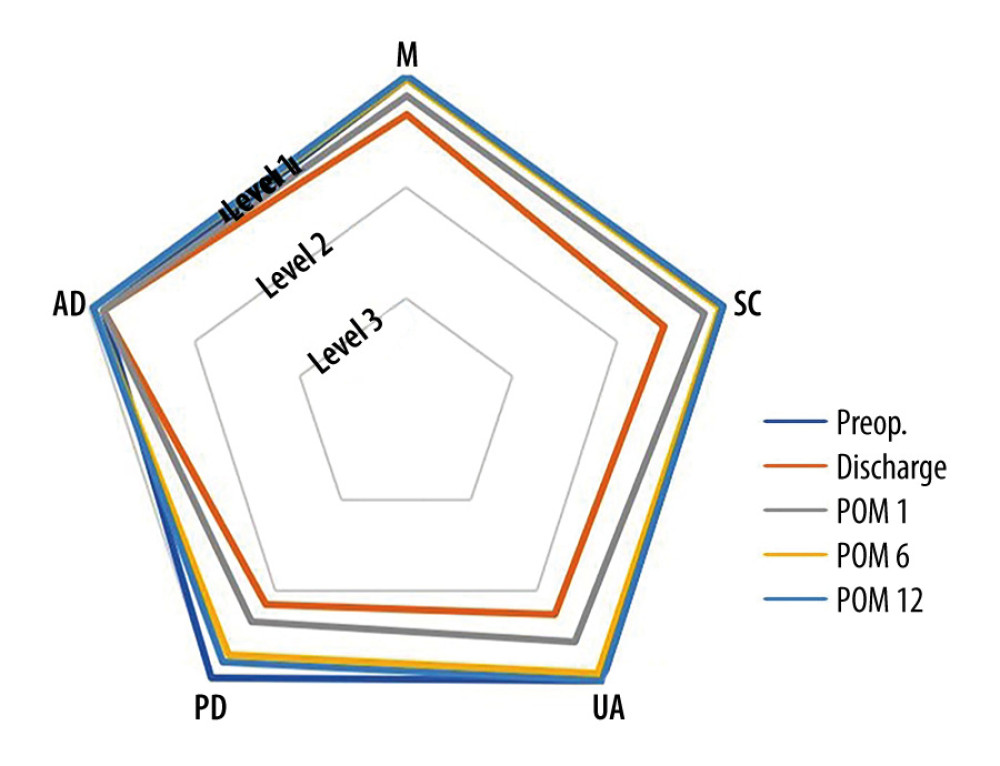 Figure 4. Mean levels of 5 dimensions according to each time of survey in EQ-5D-3L. Figure was created using Microsoft Power Point version 2019. AD – anxiety/depression; M – mobility; PD – pain/discomfort; POM – postoperative month(s); SC – self-care; UA – usual activities.
Figure 4. Mean levels of 5 dimensions according to each time of survey in EQ-5D-3L. Figure was created using Microsoft Power Point version 2019. AD – anxiety/depression; M – mobility; PD – pain/discomfort; POM – postoperative month(s); SC – self-care; UA – usual activities. 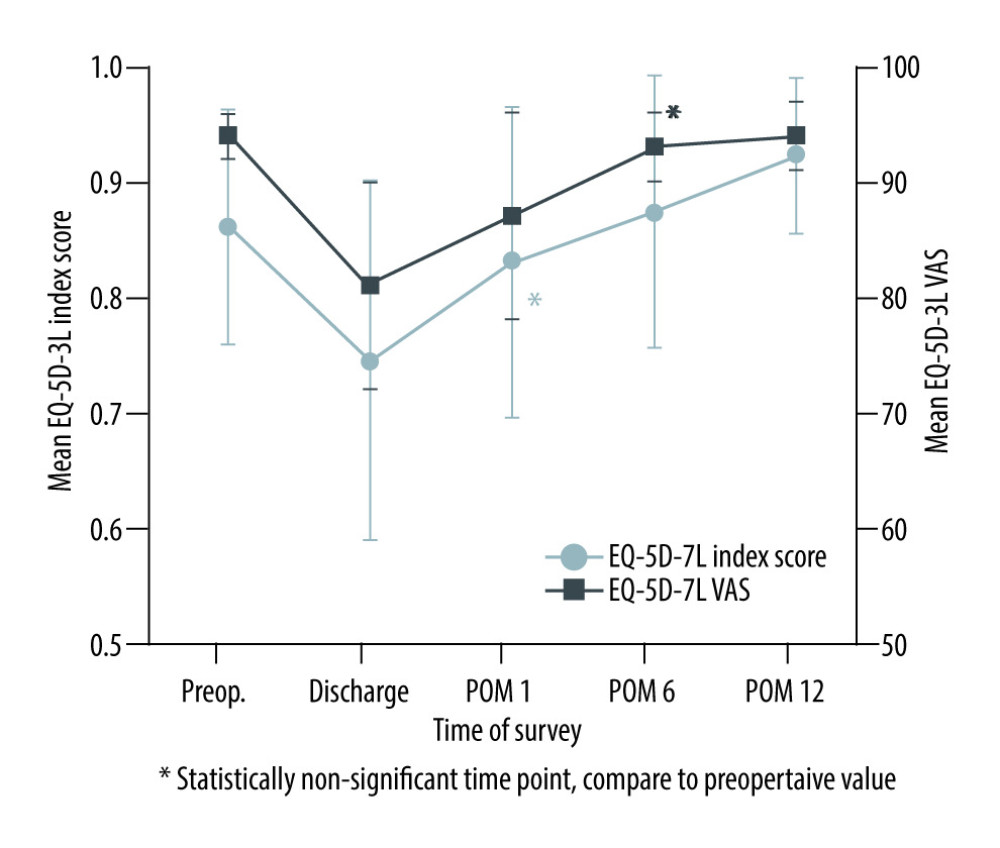 Figure 5. Mean EQ-5D-3L index score and VAS at the time of survey in 45 live liver donors who underwent LDH. Figure was created using Microsoft Power Point version 2019. LDH – laparoscopic donor hepatectomy; POM – postoperative month(s); VAS – visual analogue scale.
Figure 5. Mean EQ-5D-3L index score and VAS at the time of survey in 45 live liver donors who underwent LDH. Figure was created using Microsoft Power Point version 2019. LDH – laparoscopic donor hepatectomy; POM – postoperative month(s); VAS – visual analogue scale. Tables
Table 1. Applying the EQ-5D-3L value set for South Korea to calculate EQ-5D index score [16].![Applying the EQ-5D-3L value set for South Korea to calculate EQ-5D index score [16].](https://jours.isi-science.com/imageXml.php?i=t1-anntransplant-27-e935611.jpg&idArt=935611&w=1000) Table 2. Demographic, surgical, and postoperative factors of 47 live liver donors who underwent donor hepatectomy.
Table 2. Demographic, surgical, and postoperative factors of 47 live liver donors who underwent donor hepatectomy. Table 3. Numbers and proportions reporting levels within EQ-5D dimensions in 45 live liver donors before and after PLDH for LDLT.
Table 3. Numbers and proportions reporting levels within EQ-5D dimensions in 45 live liver donors before and after PLDH for LDLT.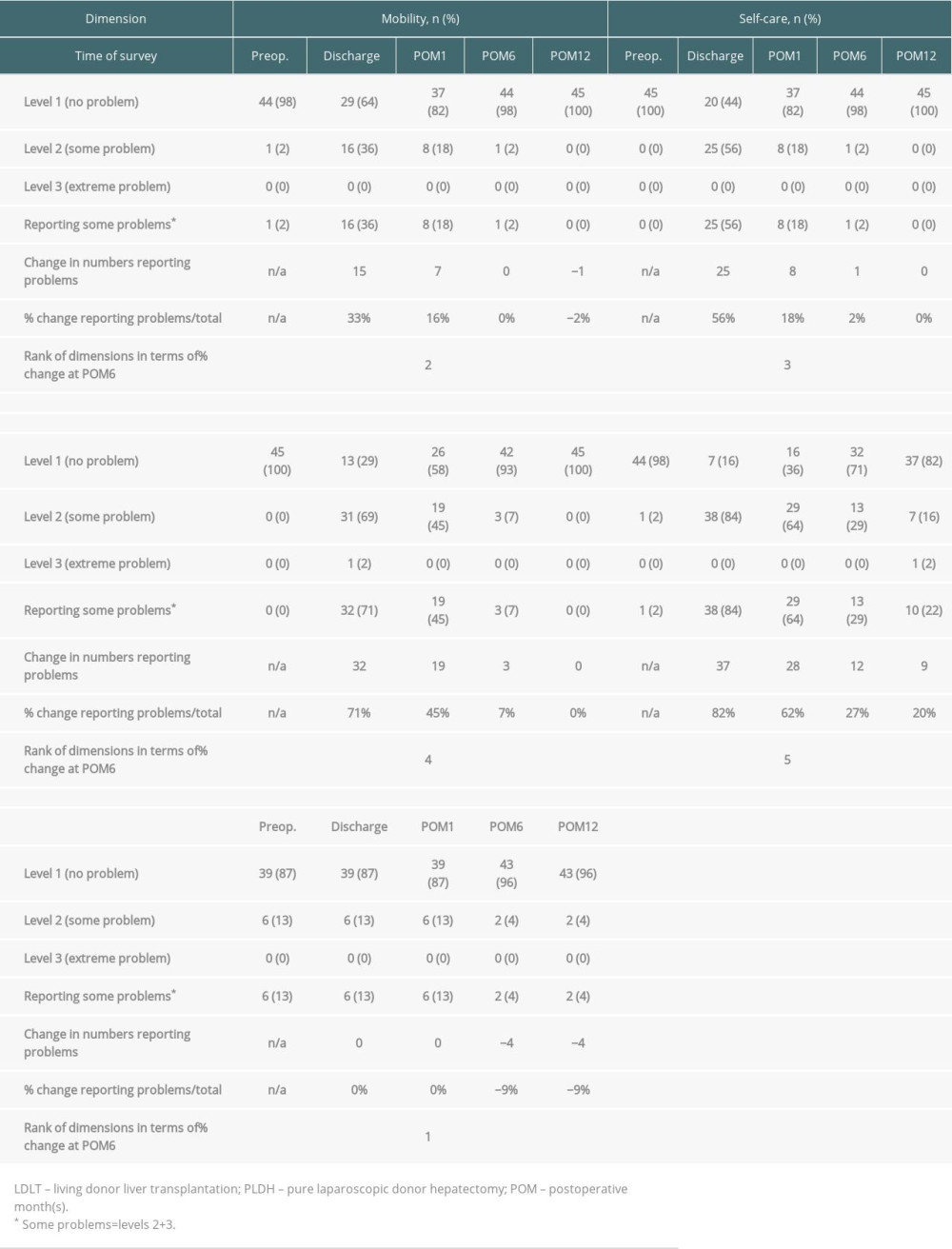
References
1. Cheah YL, Simpson MA, Pomposelli JJ, Pomfret EA, Incidence of death and potentially life-threatening near-miss events in living donor hepatic lobectomy: A world-wide survey: Liver Transpl, 2013; 19(5); 499-506
2. Hong SK, Choe S, Yi NJ, Long-term survival of 10,116 Korean live liver donors: Ann Surg, 2021; 274(2); 375-82
3. Parikh ND, Ladner D, Abecassis M, Butt Z, Quality of life for donors after living donor liver transplantation: A review of the literature: Liver Transpl, 2010; 16(12); 1352-58
4. Wakabayashi G, Cherqui D, Geller DA, Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka: Ann Surg, 2015; 261(4); 619-29
5. Ciria R, Cherqui D, Geller DA, Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing: Ann Surg, 2016; 263(4); 761-77
6. Cherqui D, Soubrane O, Husson E, Laparoscopic living donor hepatectomy for liver transplantation in children: Lancet, 2002; 359(9304); 392-96
7. Kwon CHD, Choi GS, Joh JW, Laparoscopic right hepatectomy for living donor: Curr Opin Organ Transplant, 2019; 24(2); 167-74
8. McCulloch P, Altman DG, Campbell WB, No surgical innovation without evaluation: The IDEAL recommendations: Lancet, 2009; 374(9695); 1105-12
9. Lee KW, Hong SK, Suh KS, One hundred fifteen cases of pure laparoscopic living donor right hepatectomy at a single center: Transplantation, 2018; 102(11); 1878-84
10. Rhu J, Choi GS, Kim JM, Joh JW, Kwon CHD, Feasibility of total laparoscopic living donor right hepatectomy compared with open surgery: Comprehensive review of 100 cases of the initial stage: J Hepatobiliary Pancreat Sci, 2020; 27(1); 16-25
11. Song JL, Yang J, Wu H, Pure laparoscopic right hepatectomy of living donor is feasible and safe: A preliminary comparative study in China: Surg Endosc, 2018; 32(11); 4614-23
12. Wong-Lun-Hing EM, van Dam RM, van Breukelen GJ, Randomized clinical trial of open versus laparoscopic left lateral hepatic sectionectomy within an enhanced recovery after surgery programme (ORANGE II study): Br J Surg, 2017; 104(5); 525-35
13. Morrison TG, Kalin R, Morrison MA, Body-image evaluation and body-image investment among adolescents: A test of sociocultural and social comparison theories: Adolescence, 2004; 39(155); 571-92
14. Polle SW, Dunker MS, Slors JF, Body image, cosmesis, quality of life, and functional outcome of hand-assisted laparoscopic versus open restorative proctocolectomy: Long-term results of a randomized trial: Surg Endosc, 2007; 21(8); 1301-7
15. Rabin R, de Charro F, EQ-5D: A measure of health status from the EuroQol Group: Ann Med, 2001; 33(5); 337-43
16. Lee YK, Nam HS, Chuang LH, South Korean time trade-off values for EQ-5D health states: Modeling with observed values for 101 health states: Value Health, 2009; 12(8); 1187-93
17. Rhu J, Kim MS, Choi GS, Laparoscopic living donor right hepatectomy regarding the anatomical variation of the portal vein: a propensity score-matched analysis: Liver Transpl, 2021; 27(7); 984-96
18. Zhang W, Xu L, Zhang J, Che X, Safety and feasibility of laparoscopic living donor right hepatectomy for adult liver transplantation: A meta-analysis: HPB (Oxford), 2021; 23(3); 344-58
19. Rhu J, Choi GS, Kwon CHD, Kim JM, Joh JW, Learning curve of laparoscopic living donor right hepatectomy: Br J Surg, 2020; 107(3); 278-88
20. Park J, Kwon DCH, Choi GS, Safety and risk factors of pure laparoscopic living donor right hepatectomy: Comparison to open technique in propensity score-matched analysis: Transplantation, 2019; 103(10); e308-16
21. Kwon CHD, Choi GS, Kim JM, Laparoscopic donor hepatectomy for adult living donor liver transplantation recipients: Liver Transpl, 2018; 24(11); 1545-53
22. Humphreville VR, Radosevich DM, Humar A, Longterm health-related quality of life after living liver donation: Liver Transpl, 2016; 22(1); 53-62
23. Takada Y, Suzukamo Y, Oike F, Long-term quality of life of donors after living donor liver transplantation: Liver Transpl, 2012; 18(11); 1343-52
24. Ladner DP, Dew MA, Forney S, Long-term quality of life after liver donation in the adult to adult living donor liver transplantation cohort study (A2ALL): J Hepatol, 2015; 62(2); 346-53
25. Ispir M, Cumhur B, Sahin T, Psychosocial outcomes of donors whose recipients died after living donor liver transplantation: J Gastrointest Cancer, 2020; 51(4); 1200-8
26. Kim-Schluger L, Florman SS, Schiano T, Quality of life after lobectomy for adult liver transplantation: Transplantation, 2002; 73(10); 1593-97
27. Karliova M, Malago M, Valentin-Gamazo C, Living-related liver transplantation from the view of the donor: A 1-year follow-up survey: Transplantation, 2002; 73(11); 1799-804
28. Feltrin A, Pegoraro R, Rago C, Experience of donation and quality of life in living kidney and liver donors: Transpl Int, 2008; 21(5); 466-72
29. Verbesey JE, Simpson MA, Pomposelli JJ, Living donor adult liver transplantation: A longitudinal study of the donor’s quality of life: Am J Transplant, 2005; 5(11); 2770-77
30. Chan SC, Liu CL, Lo CM, Donor quality of life before and after adult-to-adult right liver live donor liver transplantation: Liver Transpl, 2006; 12(10); 1529-36
31. Brazier J, Roberts J, Deverill M, The estimation of a preference-based measure of health from the SF-36: J Health Econ, 2002; 21(2); 271-92
32. Rowen D, Brazier J, Roberts J, Mapping SF-36 onto the EQ-5D index: How reliable is the relationship?: Health Qual Life Outcomes, 2009; 7; 27
Figures
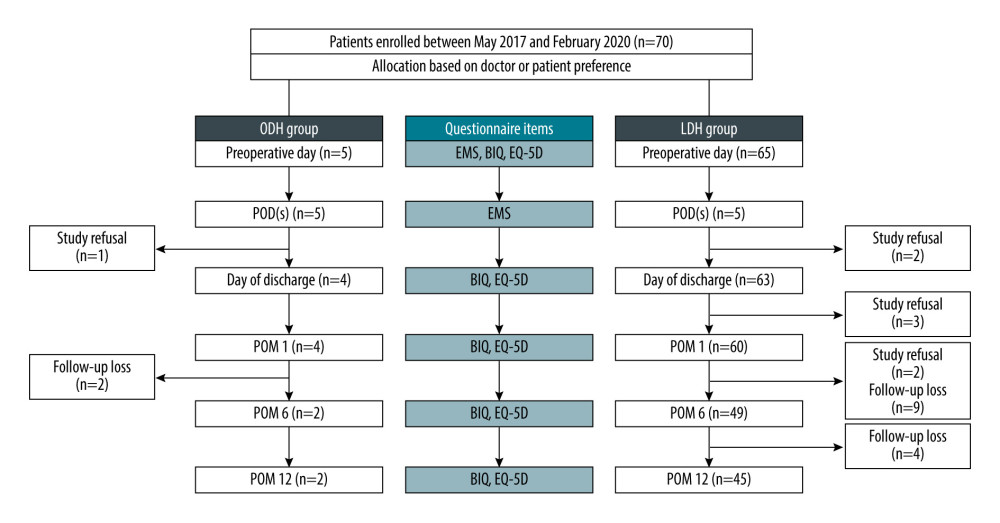 Figure 1. Study flow chart. Figure was created using Microsoft Power Point version 2019. BIQ – Body Image Questionnaire; EMS – ERAS mobility score; LDH – laparoscopic donor hepatectomy; ODH – open donor hepatectomy; POD – postoperative day(s); POM – postoperative month(s).
Figure 1. Study flow chart. Figure was created using Microsoft Power Point version 2019. BIQ – Body Image Questionnaire; EMS – ERAS mobility score; LDH – laparoscopic donor hepatectomy; ODH – open donor hepatectomy; POD – postoperative day(s); POM – postoperative month(s).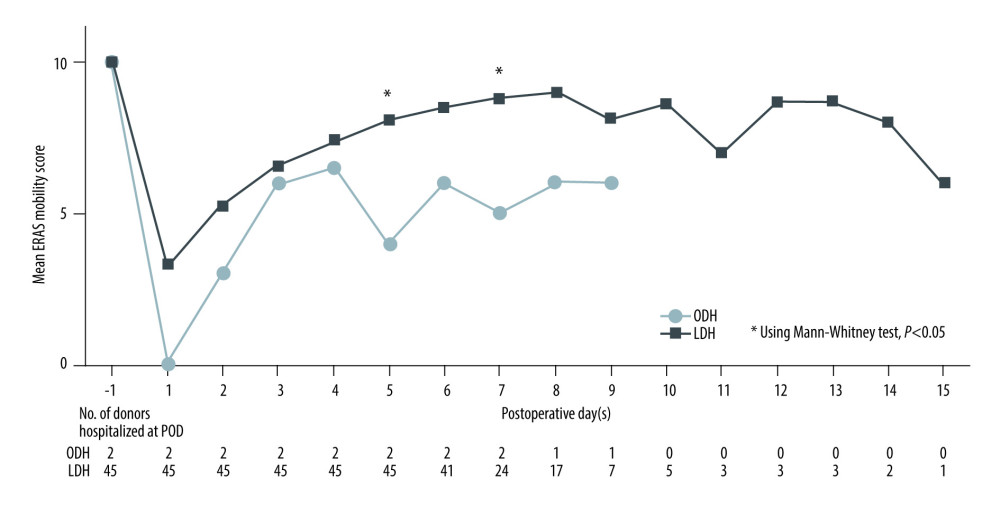 Figure 2. Mean ERAS mobility score between the ODH and LDH groups during hospitalization after DH. Figure was created using Microsoft Power Point version 2019. LDH, laparoscopic donor hepatectomy; ODH, open donor hepatectomy; POD, postoperative day(s).
Figure 2. Mean ERAS mobility score between the ODH and LDH groups during hospitalization after DH. Figure was created using Microsoft Power Point version 2019. LDH, laparoscopic donor hepatectomy; ODH, open donor hepatectomy; POD, postoperative day(s).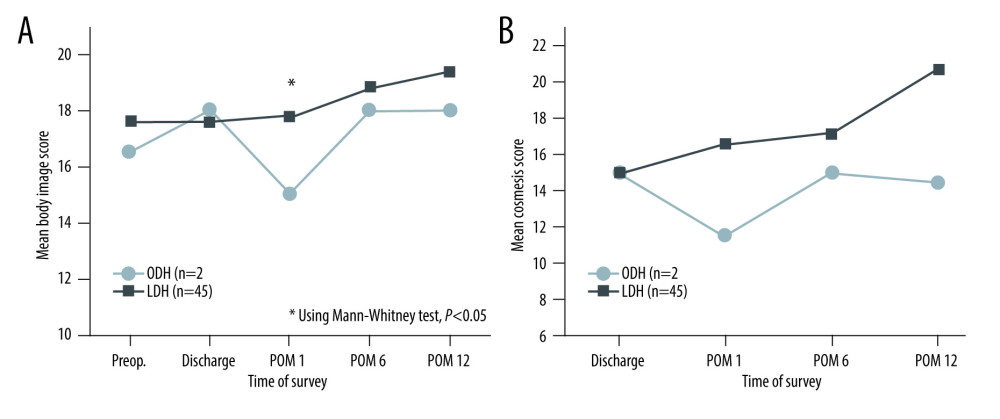 Figure 3. Mean body image score (A) and cosmesis score (B) between the ODH and LDH groups. Figure was created using Microsoft Power Point version 2019. LDH – laparoscopic donor hepatectomy; ODH – open donor hepatectomy; POM – postoperative month(s).
Figure 3. Mean body image score (A) and cosmesis score (B) between the ODH and LDH groups. Figure was created using Microsoft Power Point version 2019. LDH – laparoscopic donor hepatectomy; ODH – open donor hepatectomy; POM – postoperative month(s).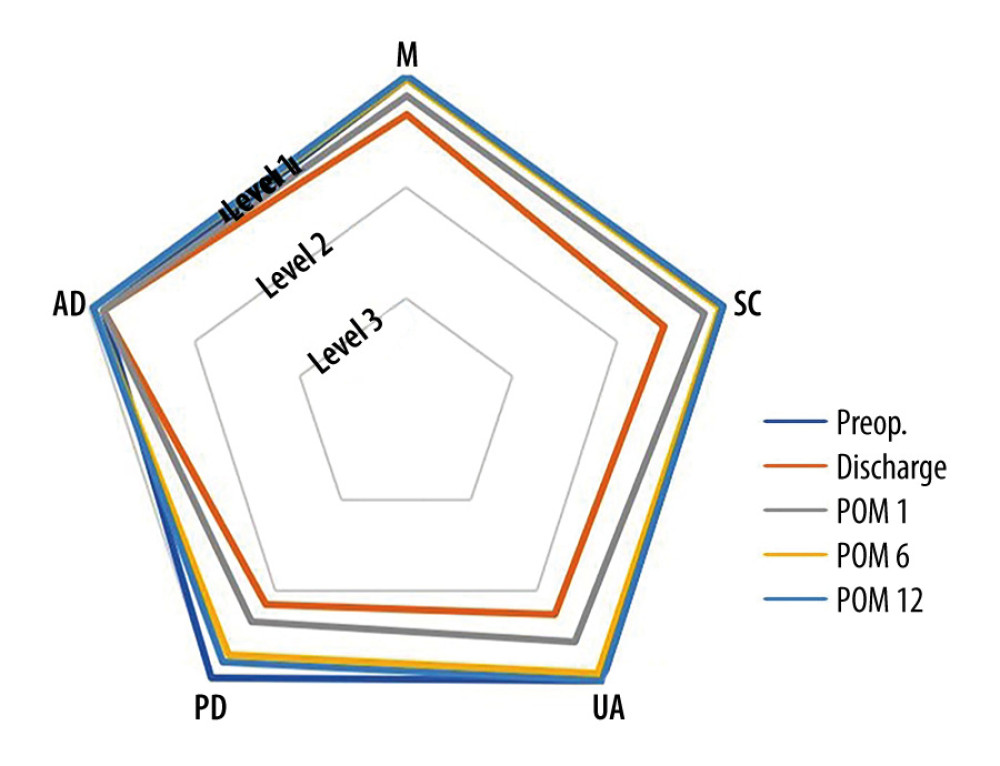 Figure 4. Mean levels of 5 dimensions according to each time of survey in EQ-5D-3L. Figure was created using Microsoft Power Point version 2019. AD – anxiety/depression; M – mobility; PD – pain/discomfort; POM – postoperative month(s); SC – self-care; UA – usual activities.
Figure 4. Mean levels of 5 dimensions according to each time of survey in EQ-5D-3L. Figure was created using Microsoft Power Point version 2019. AD – anxiety/depression; M – mobility; PD – pain/discomfort; POM – postoperative month(s); SC – self-care; UA – usual activities.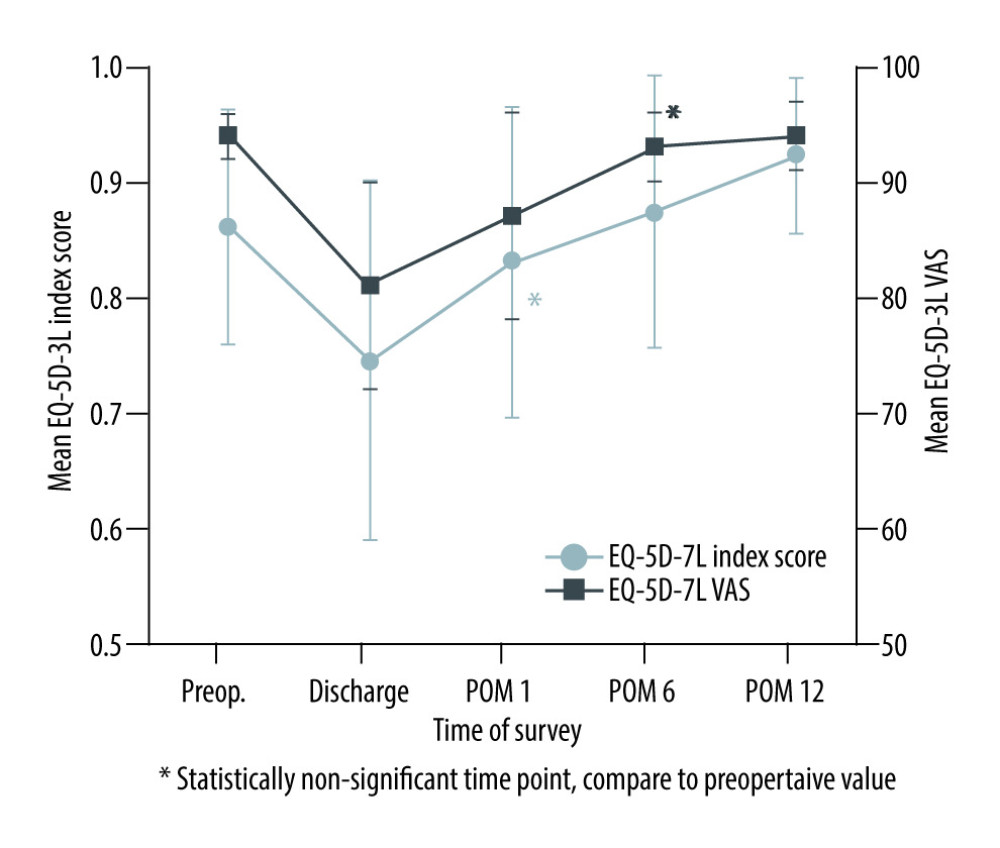 Figure 5. Mean EQ-5D-3L index score and VAS at the time of survey in 45 live liver donors who underwent LDH. Figure was created using Microsoft Power Point version 2019. LDH – laparoscopic donor hepatectomy; POM – postoperative month(s); VAS – visual analogue scale.
Figure 5. Mean EQ-5D-3L index score and VAS at the time of survey in 45 live liver donors who underwent LDH. Figure was created using Microsoft Power Point version 2019. LDH – laparoscopic donor hepatectomy; POM – postoperative month(s); VAS – visual analogue scale. Tables
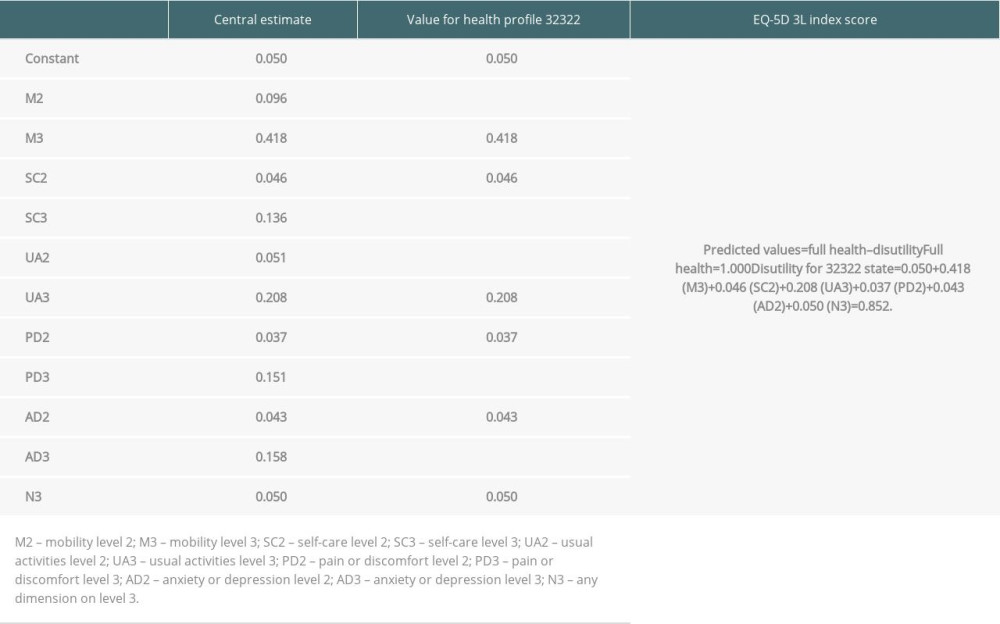 Table 1. Applying the EQ-5D-3L value set for South Korea to calculate EQ-5D index score [16].
Table 1. Applying the EQ-5D-3L value set for South Korea to calculate EQ-5D index score [16]. Table 2. Demographic, surgical, and postoperative factors of 47 live liver donors who underwent donor hepatectomy.
Table 2. Demographic, surgical, and postoperative factors of 47 live liver donors who underwent donor hepatectomy.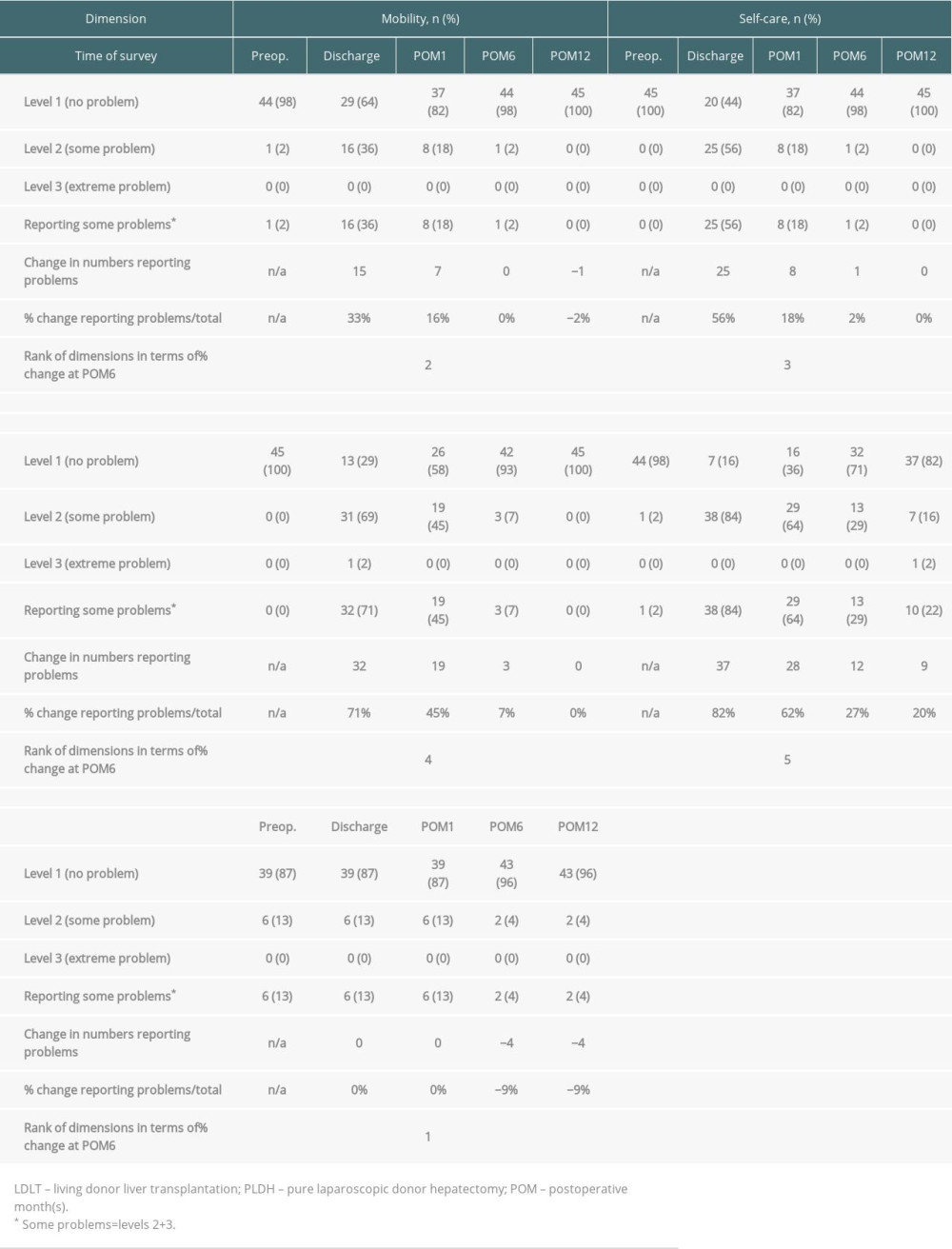 Table 3. Numbers and proportions reporting levels within EQ-5D dimensions in 45 live liver donors before and after PLDH for LDLT.
Table 3. Numbers and proportions reporting levels within EQ-5D dimensions in 45 live liver donors before and after PLDH for LDLT.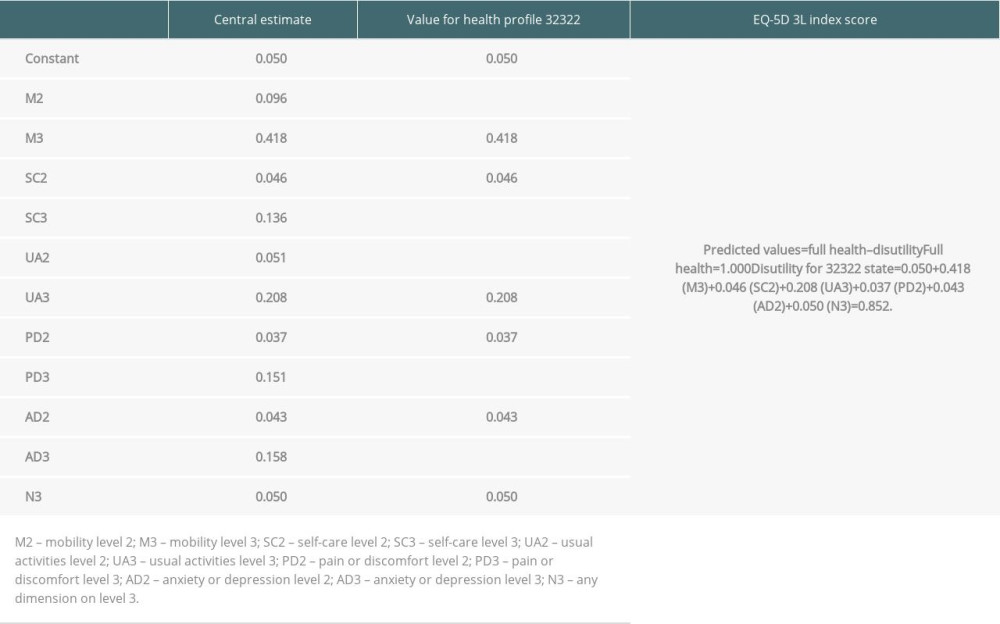 Table 1. Applying the EQ-5D-3L value set for South Korea to calculate EQ-5D index score [16].
Table 1. Applying the EQ-5D-3L value set for South Korea to calculate EQ-5D index score [16]. Table 2. Demographic, surgical, and postoperative factors of 47 live liver donors who underwent donor hepatectomy.
Table 2. Demographic, surgical, and postoperative factors of 47 live liver donors who underwent donor hepatectomy.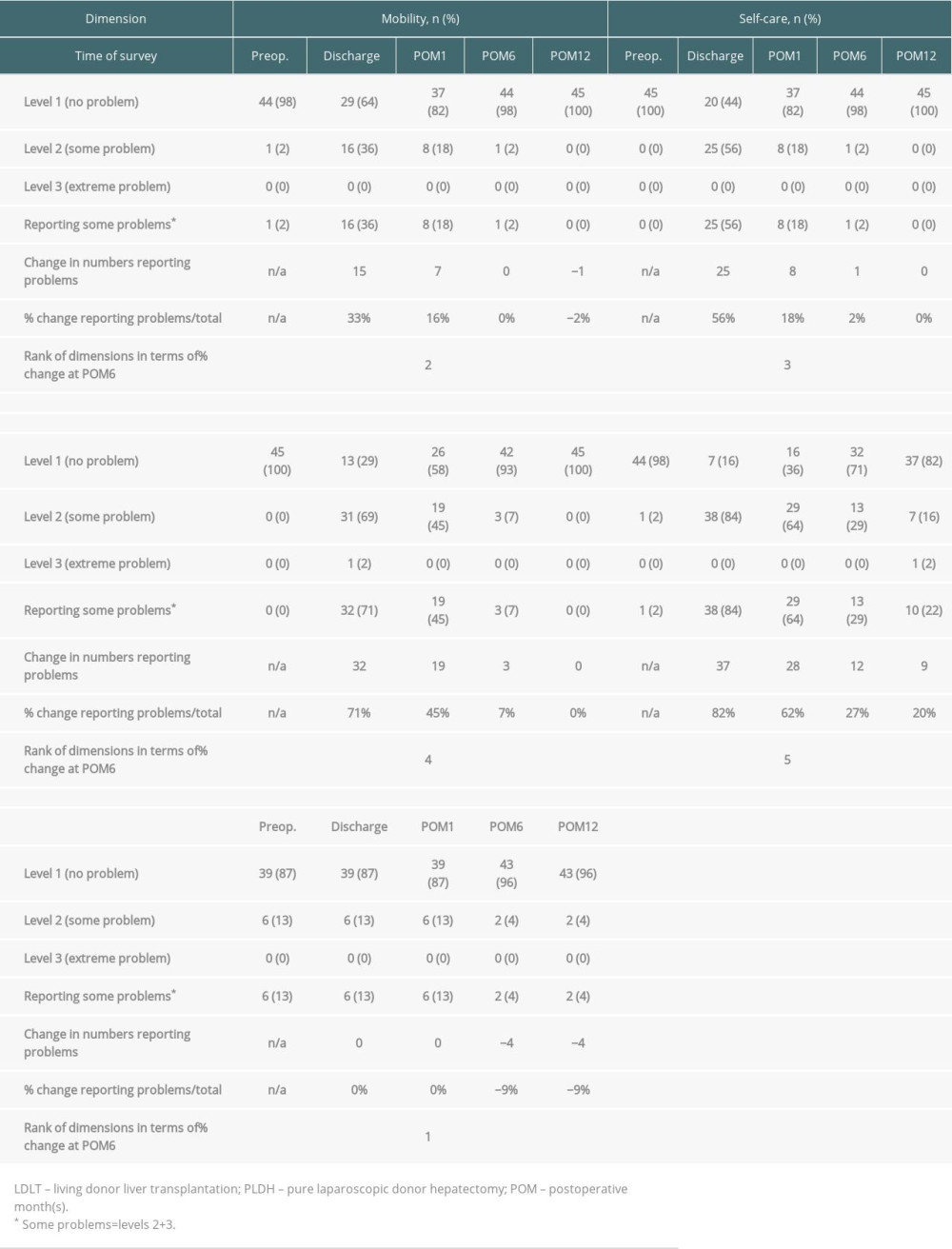 Table 3. Numbers and proportions reporting levels within EQ-5D dimensions in 45 live liver donors before and after PLDH for LDLT.
Table 3. Numbers and proportions reporting levels within EQ-5D dimensions in 45 live liver donors before and after PLDH for LDLT. In Press
15 Mar 2024 : Review article
Approaches and Challenges in the Current Management of Cytomegalovirus in Transplant Recipients: Highlighti...Ann Transplant In Press; DOI: 10.12659/AOT.941185
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








