15 September 2020: Original Paper
Evaluation of the Effectiveness of Screening for Iliac Arterial Calcification in Kidney Transplant Candidates
Stephanie A. DeBolle1ABCDEFG*, Ivy A. Ochieng1BCDEF, Anjan K. Saha1CDE, Randall S. Sung1ABCDEFDOI: 10.12659/AOT.922178
Ann Transplant 2020; 25:e922178
Abstract
BACKGROUND: Peripheral vascular disease and iliac arterial calcification are prevalent in kidney transplant candidates and jeopardize graft outcomes. We report our experience with computed tomography (CT) screening for iliac arterial calcification.
MATERIAL AND METHODS: We retrospectively reviewed electronic medical records of 493 renal transplant candidates from protocol initiation in 2014. Non-contrast CT was performed or retrospectively reviewed if any of the following criteria were present: diabetes, ESRD >6 years, 25 pack-years of smoking or current smoker, diagnosis of peripheral vascular disease, parathyroidectomy, and coronary artery disease intervention. Differences in evaluation and transplant outcomes between groups were compared with chi-squared analysis. Multivariate logistic regression identified predictive criteria for presence of iliac arterial calcification.
RESULTS: Of 493 candidates evaluated, CTs were reviewed in 346 (70.2%). Iliac arterial calcification was identified in 119 screened candidates (34.4%). Of candidates with iliac arterial calcification identified on CT, 16 (13.4%) were excluded for CT findings, and 9 (7.6%) had their surgical management plan changed. Overall, 91 (76.5%) candidates with iliac arterial calcification on CT were approved, compared to 203 (89.4%) without calcification (P<0.001). The percentage of screened patients with iliac arterial calcification on CT increased with increasing age (P<0.0005). Age and diabetes mellitus were predictive of calcification.
CONCLUSIONS: Many kidney transplant candidates are at risk for iliac arterial calcification, although such calcification does not prevent transplantation for most candidates who have it. Algorithmic pre-operative screening has clinical value in determining transplant candidacy and potentially improving postoperative outcomes in patients requiring kidney transplantation.
Keywords: Kidney Transplantation, Organ Transplantation, peripheral arterial disease, Iliac Artery, Tomography, X-Ray Computed, vascular calcification
Background
Chronic kidney disease (CKD) affects 1 in 7 adults in the United States, and over 600 000 Americans have end-stage renal disease (ESRD) [1]. Renal transplantation is the treatment of choice for patients with ESRD, and, with the waiting list far exceeding the supply of available organs, the judicious use of organs is imperative [2]. Eligibility for kidney transplant is contingent upon pre-operative evaluation that establishes treatment candidacy and can dictate peri- and postoperative care [3]. Coincident comorbidities can be primary determinants of transplant candidacy and post-transplant outcomes.
Peripheral vascular disease is a common comorbidity found in patients needing kidney transplantation [4] and is characterized by hardening and narrowing of arteries other than in the heart and brain. Peripheral vascular disease can manifest as calcific or occlusive disease [3,5]. Phenotypic plasticity of vascular cells that recapitulates embryonic endochondral ossification is thought to drive vascular calcification by way of bone morphogenetic proteins that are triggered and modulated by a number of inflammatory, metabolic, and genetic disorders [6,7]. Vascular calcification is very common in CKD patients; in fact, the most extensive vascular calcification occurs in patients with CKD [6].
Although peripheral vascular disease is very prevalent among patients with ESRD, it is often underdiagnosed in this patient population [4]. However, its identification in transplant patients is essential because of the known adverse relationship between peripheral vascular disease and transplant outcomes. Lower extremity peripheral arterial disease is associated with lower patient survival after renal transplantation, and moderate-to-severe lower extremity arterial calcification is associated with increased waitlist mortality and lower patient and graft survival after transplantation [4,8,9]. Peripheral vascular disease is also one of the core parameters utilized in preoperative risk stratification indexes for mortality prediction in transplant candidates [10]. It has also been associated with significant coronary vascular disease requiring coronary intervention prior to renal transplantation [11]. Surgically, peripheral vascular disease of the iliac arteries jeopardizes patient outcomes owing to either compromised inflow to the transplanted kidney or implantation failure due to vessel calcification. While occlusive disease can be identified clinically, calcific disease is often silent. There is currently no consensus on the most appropriate technique to diagnose vascular calcification in patients with CKD [12,13].
We recently implemented a computed tomography (CT) scan screening protocol for the detection and characterization of iliac arterial calcification in patients with CKD. To better understand this patient population, we assessed the pre-screening attributes of an internal cohort of patients before and after implementation of the screening protocol. We characterized post-screening clinical decision making from a systems level perspective and further identified factors within the established pre-screening parameters that were significantly associated with a positive CT scan for iliac arterial calcification. The aims of this study are to inform similarly sized health systems of the effectiveness of preoperative screening and to identify the subset of patients most likely to benefit from such screening.
Material and Methods
This was a single-center retrospective observational study of patients evaluated for renal transplantation. We retrospectively reviewed the electronic medical records of 1092 renal allograft candidates from 2007 to 2015 at the University of Michigan Health System. Starting in 2014, transplant candidates, including those already listed or previously evaluated, were screened for iliac arterial calcification by non-contrast CT scan. Institutional Review Board approval was obtained, and the study was exempt for approval from an ethics board. Those with signs and symptoms of occlusive disease received contrast CT where indicated. While venous disease could be identified in the CT scan assessment, the protocol was specifically designed to address peripheral arterial disease, and more specifically calcification.
The screening criteria included: 1) history or symptoms of occlusive disease: claudication, rest pain, presence of non-healing ulcer(s), diminished femoral pulses, or calcified vessels on physical exam; 2) ESRD for more than 6 years; 3) currently smoking or history of more than 25 pack-years; 4) diabetes mellitus; 5) intervention for coronary artery disease; and 6) parathyroidectomy (hyperparathyroidism is a risk factor for peripheral vascular calcification) [14].
Patients who qualified for screening based on the above criteria underwent a non-contrast CT scan to identify iliac artery calcifications. All CTs were reviewed by a transplant surgeon. Degree of calcification was defined as: no disease: calcification in the iliac arteries is absent or minimal; moderate disease: calcification is limited to the common iliac artery or, if present in the external iliac artery, does not affect ability to occlude the artery or perform anastomosis; and severe disease: calcification is significant enough to anticipate requiring either anastomosis or clamping in calcified areas, or prohibits transplant altogether.
Candidates could have been excluded based on CT findings alone, or in consideration of overall risk. Patients with potentially significant iliac occlusive disease were either worked up further with noninvasive flow studies or referred to a vascular surgeon.
We identified 493 patients who met the above criteria and were screened using the new protocol; reasons for screening were recorded (Figure 1). Patients were excluded if they had previous transplants, did not meet the screening criteria, or had an incomplete medical record. Of the total patients, 346 had CT scans evaluated for iliac arterial calcification and were classified based on severity or extent of calcification on CT, as described above. Data were recorded on transplant acceptance and whether non-acceptance was attributable to CT findings. The primary outcome measures were identification of calcification and the ability of the screening protocol to predict calcification. Secondary outcomes were the impact of CT findings on either transplant candidacy or operative approach (i.e., whether the CT findings directed either laterality of the recipient operation or specified the target artery).
Differences between groups were compared with chi-squared analysis for categorical variables. Multivariate logistic regression analysis was conducted to identify significant associations between the eligibility criteria and the identification of moderate or severe disease.
Results
Table 1 shows the number of patients that matched each criterion, as well as the number of patients screened, their screening outcomes, and whether management was changed as a result of CT findings. Diabetes was the most common criterion in candidates who qualified for screening and in those screened. However, iliac arterial calcification was most frequently identified in those candidates who had smoking and coronary artery disease intervention as screening criteria, and these patients were most frequently ruled out owing to severity of disease. Table 2 highlights the demographics of this cohort.
Of the patients that qualified for screening, 379 (nearly 80%) met only 1 or 2 of the criteria, and a small proportion met several (Figure 2). Of the 346 patients screened with a CT scan, 119 patients (34.4%) were found to have iliac arterial calcification on CT; 77 had moderate disease; and 42 had severe disease. These patients were divided into age groups (Figure 3), and a significant association (
Of the 119 patients with iliac arterial calcification, 91 (76.5%) were accepted for transplant listing, compared to the 203 of 227 patients (89.4%) without calcification that were accepted (
Looking further into each screening criterion, we found that no patients were ruled out owing to iliac arterial calcification on CT when the only criterion they met was either ESRD >6 years or parathyroidectomy. Among the 124 patients with ESRD >6 years, 38 met no other screening criteria, and among this subgroup no patients were ruled out because of iliac arterial calcification. Among the 21 patients with a history of a parathyroidectomy, 5 met no other screening criteria and none were ruled out because of iliac arterial calcification in this subgroup. All other screening criteria resulted in the unique identification of calcification that resulted in patients being ruled out for transplant candidacy.
We conducted multivariate regression analysis to identify the screening criteria that were most likely to be associated with iliac arterial calcification on CT. Gender, age, race, and BMI were included with the protocol screening criteria in the full model. Age and diabetes were significantly associated with iliac arterial calcification on CT, corroborating earlier findings that older patients in this screened population were more likely to exhibit iliac arterial calcification on CT (Table 4).
Discussion
Ensuring the long-term success of renal transplantation is critical to maintaining the capacity of health systems to manage the increasing burden of ESRD. Given the rising demand for organ transplantation, predictive algorithms that can identify candidates with a lower likelihood of developing short- and long-term complications will be instrumental in facilitating the judicious allocation of resources. Iliac arterial calcification is important because it can negatively affect transplant outcome. Imaging modalities such as CT and X-ray that screen for vascular calcification have an essential role in informing mortality risk and therapeutic approaches in patients with CKD [15]. Here, we report the implementation of a novel screening protocol that leverages CT scans to identify calcific/occlusive disease in high-risk renal transplant candidates.
As is common with new protocols, we had a transition period before full implementation. As such, of the 493 patients that qualified for the screening protocol, 346 (70.2%) underwent CT scanning. For those who underwent screening, our results showed concordance between the extent of calcific disease found on CT scan and the proportion of patients who were ruled out not only for this disease but for any cause. Intriguingly, a majority of these patients were ruled out for reasons other than calcific disease, demonstrating either that iliac calcification on CT acted as a surrogate for poor transplant candidacy or that the additional risk of calcification was a contributory factor in otherwise marginal candidates. Furthermore, the protocol identified 16 patients with calcific disease that was too extensive to be considered for transplantation listing regardless of other risks.
Among the 6 screening criteria, the magnitude of associations with iliac arterial calcification identification varied. Logistic regression analysis demonstrated that, of the 6 criteria, only diabetic status was significantly associated with calcification. To understand the importance of each criterion’s associations with calcification, we isolated each criterion and looked at the patients that qualified for screening based on that criterion alone. We found that among patients qualifying because of either ESRD >6 years or history of parathyroidectomy alone, no patients were ruled out because of iliac arterial calcification. Hence, despite evidence that suggested increased risk of arterial calcification in these patients, we did not find this to be indicative of iliac calcification in our population, and thus we removed these criteria from the screening protocol.
Age was highly associated with arterial calcification in this study, which is consistent with prior work showing that the prevalence of coronary calcification rises with advancing age [4]. While age is a known risk factor for peripheral arterial disease and coronary calcification, it is important to remember that this is a screened population with other risk factors for calcification (diabetes, coronary artery disease, smoking, ESRD vintage), and age is not necessarily a priori associated with clinically significant iliac arterial calcification, as defined by this study in this population. Indeed, our experience with CT reviews performed outside of this protocol in candidates who did not meet screening criteria suggest that age alone should not be included in the absence of other risk factors. However, our results do suggest that screening is not necessary in any candidate under age 35, regardless of other risks, as no patient under age 35 was found to have iliac arterial calcification on CT.
Of the patients screened for iliac arterial calcification using CT scanning, 9 patients (2.6%) underwent a change in transplant laterality or in the vessel used for transplant owing to findings in the CT scan. This demonstrates that the protocol, in addition to finding high-risk candidates, can be used to better individualize surgical approach.
While our screening protocol appears to have measurable benefits, several limitations impacted the conclusions of our study. Many patients were not included in the analyses because of incomplete medical history. Not all patients that met criteria were imaged, which is a logistical consideration to be further evaluated and addressed. The scale used to classify the extent of calcification on the CT scans was a subjective scale rather than an objective scale. Operator dependency is a widely accepted source of inconsistency when evaluating radiographic findings, and having varying physicians label the extent of calcification may have introduced heterogeneity into the results. Therefore, our findings may have limited statistical power owing to exclusion, incomplete screening implementation, and operator inconsistency in the determination of the extent of calcific disease.
The number of patients that have undergone the screening protocol and gone on to be transplanted is low given the recent implementation of the protocol, and thus additional time and patient volume will improve the power of our analyses. Above and beyond determining surgical candidacy, the utilization of CT indicators of the overall burden of calcification may further inform outcomes, given the previously reported associations with cardiovascular events and mortality in dialysis patients [12,16].
Conclusions
The impact of iliac arterial calcification on renal transplantation is significant. Our findings after the initial implementation of a novel protocol utilizing CT scanning for screening of iliac arterial calcification show promise to improve transplant patient selection. The protocol helped to rule out candidates with extensive disease or identified patients that were ruled out for additional reasons. Therefore, the protocol successfully helped identify less suitable transplant candidates with higher risk of adverse outcomes and complications, many of whom may have experienced an aborted transplant operation in the absence of screening. The sub-analysis of each screening criteria identified possible enhancements to the protocol, namely, to exclude patients under the age of 35, and to include only 4 criteria: history of diabetes mellitus, smoking status, history of coronary artery disease intervention, and history of peripheral artery disease. Though our preliminary findings support the continued use of the protocol, longitudinal data is needed to determine whether the protocol enhances transplant outcomes and if it effectively identifies patients at risk for inferior outcomes.
Figures
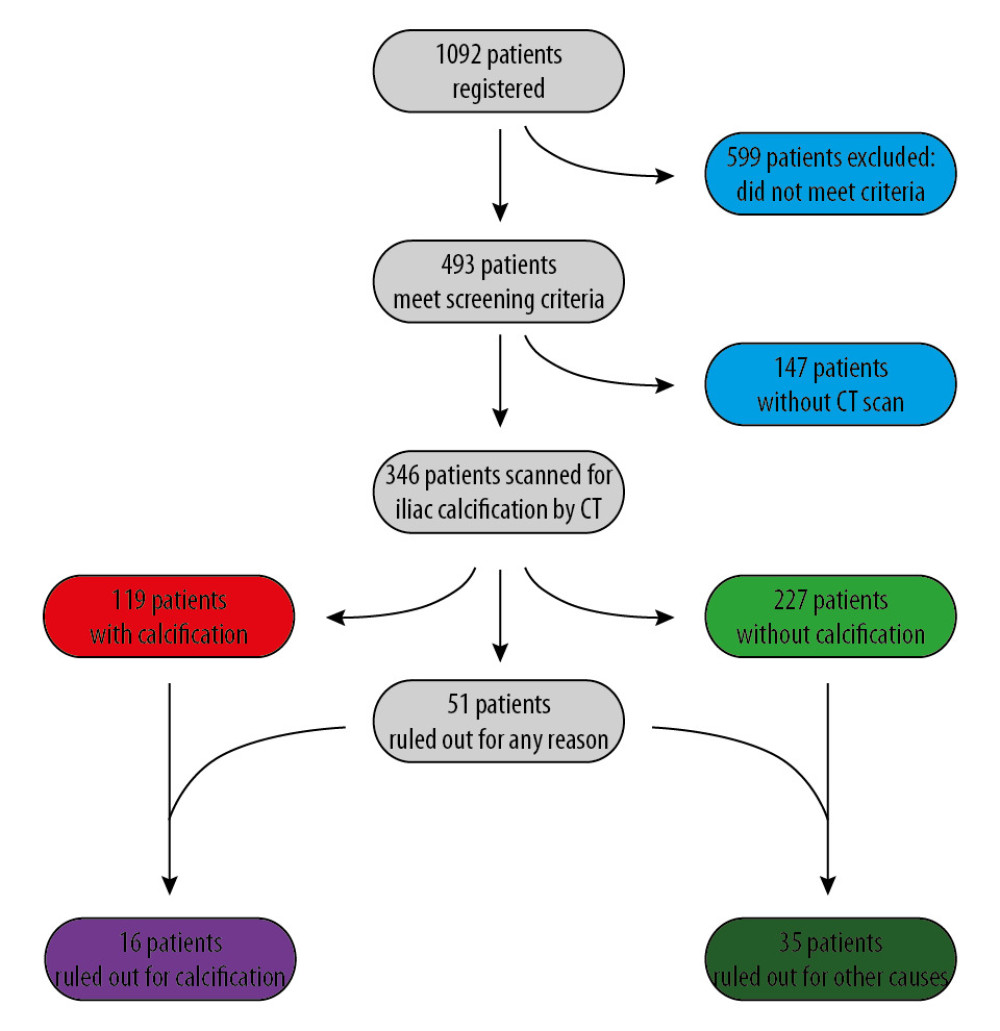 Figure 1. Study population, exclusions, outcomes of CT scanning, and candidate acceptance.
Figure 1. Study population, exclusions, outcomes of CT scanning, and candidate acceptance. 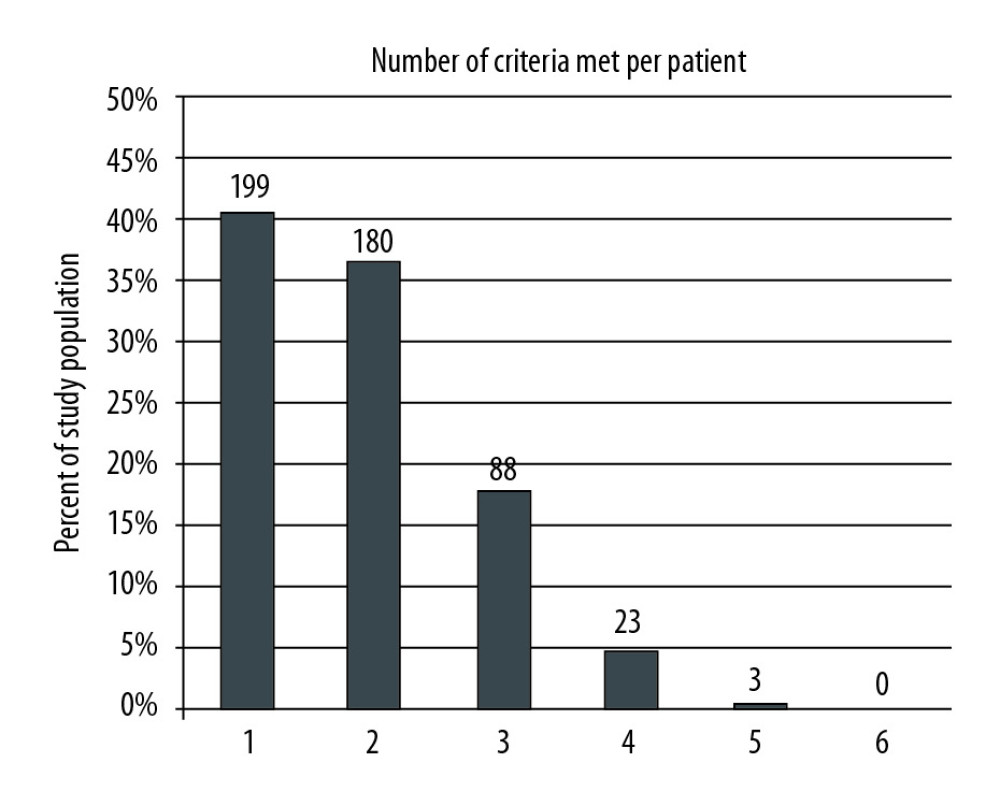 Figure 2. The patient cohort was analyzed to determine how many of the 6 screening criteria each patient met. The number of patients and percentage of the entire cohort meeting 1 through 6 of the criteria is shown. The majority of patients met 1 or 2 of the criteria.
Figure 2. The patient cohort was analyzed to determine how many of the 6 screening criteria each patient met. The number of patients and percentage of the entire cohort meeting 1 through 6 of the criteria is shown. The majority of patients met 1 or 2 of the criteria. 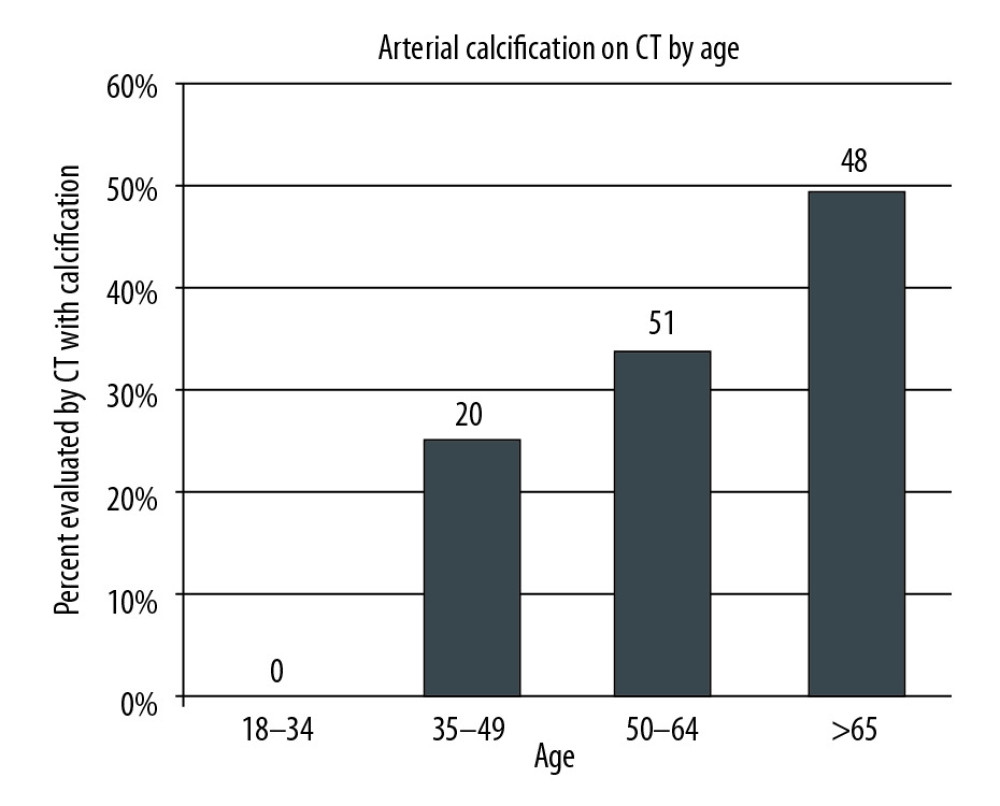 Figure 3. Age distribution of patients that were found to have iliac arterial calcification on CT scan.
Figure 3. Age distribution of patients that were found to have iliac arterial calcification on CT scan. 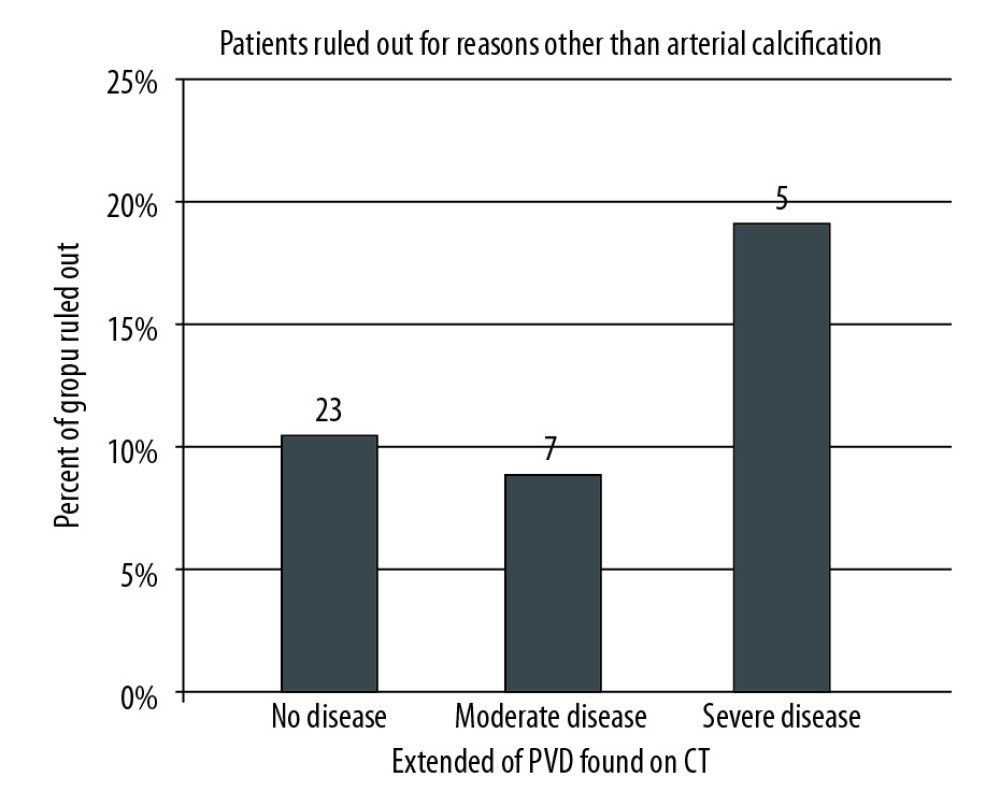 Figure 4. Patients evaluated with CT scan were categorized by the extent of iliac arterial calcification found on CT: no, moderate, or severe disease. Each group was further analyzed to determine the percentage of patients who were ruled out for other or additional reasons. Patients who were ruled out exclusively on the basis of arterial calcification were excluded from this analysis.
Figure 4. Patients evaluated with CT scan were categorized by the extent of iliac arterial calcification found on CT: no, moderate, or severe disease. Each group was further analyzed to determine the percentage of patients who were ruled out for other or additional reasons. Patients who were ruled out exclusively on the basis of arterial calcification were excluded from this analysis. References
1. NIDDK Information Clearinghouse: Kidney Disease Statistics for the United States Accessed at: https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease
2. Gang S, Rajapurkar M, Vascular complications following renal transplantation: J Nephrol Renal Transplantation, 2009; 2(1); 122-32
3. University of Michigan Transplant Center: Clinical practice guidelines for the evaluation of kidney patients September 27, 2017
4. Aitken E, Ramjug S, Buist L, Kingsmore D, The prognostic significance of iliac vessel calcification in renal transplantation: Transplant Proc, 2012; 44(10); 2925-31
5. , Medline Plus: Peripheral artery disease – legs, 2015 Available at: http://www.nlm.nih.gov/medlineplus/ency/article/000170.htm
6. Sage AP, Tintut Y, Demer LL, Regulatory mechanisms in vascular calcification: Nat Rev Cardiol, 2010; 7; 528-36
7. Zoccali C, Bolignano D, D’Arrigo GEuropean Renal and Cardiovascular Medicine (EURECA-m) Working Group of the European Renal Association-European Dialysis Transplantation Association (ERA-EDTA), Validity of vascular calcification as a screening tool and as a surrogate end point in clinical research: Hypertension, 2015; 66(1); 3-9
8. Sung RS, Althoen M, Howell TA, Merion RM, Peripheral vascular occlusive disease in renal transplant recipients: Risk factors and impact on kidney allograft survival: Transplantation, 2000; 70(7); 1049-54
9. Wu DA, Robb ML, Forsythe JLR, Recipient comorbidity and survival outcomes after kidney transplantation: Transplantation, 2019; 104(6); 1246-55
10. Park JY, Kim MH, Bae EJ, Comorbidities can predict the mortality of kidney transplant recipients: Transplantation, 2018; 50(4); 1068-73
11. Puttarajappa CM, Tevar AD, Hariharan S, Screening coronary angiography in patients with long standing diabetes mellitus undergoing kidney transplant evaluation: Clin Transplant, 2019; 33(4); e13501
12. NasrAllah MM, Nassef A, Elshaboni TH, Comparing different calcification scores to detect outcomes in chronic kidney disease patients with vascular calcification: Int J Cardiol, 2016; 220; 884-89
13. Ketteler M, Elder GJ, Ketteler P, A commentary from a Kidney Disease: Improving Global Outcomes controversies conference: Kidney Int, 2015; 87(3); 502-28
14. Brown SJ, Ruppe MD, Tabatabai LS, The parathyroid gland and heart disease: Methodist Debakey Cardiovasc J, 2017; 13(2); 49-54
15. Adragão T, Pires A, Birne R, A plain X-ray vascular calcification score is associated with arterial stiffness and mortality in dialysis patients: Nephrol Dial Transplant, 2009; 24(3); 997-1002
16. Verbeke F, Van Biesen W, Honkanen ECORD Study Investigators, Prognostic value of aortic stiffness and calcification for cardiovascular events and mortality in dialysis patients: Outcome of the calcification outcome in renal disease (CORD) study: Clin J Am Soc Nephrol, 2011; 6(1); 153-59
Figures
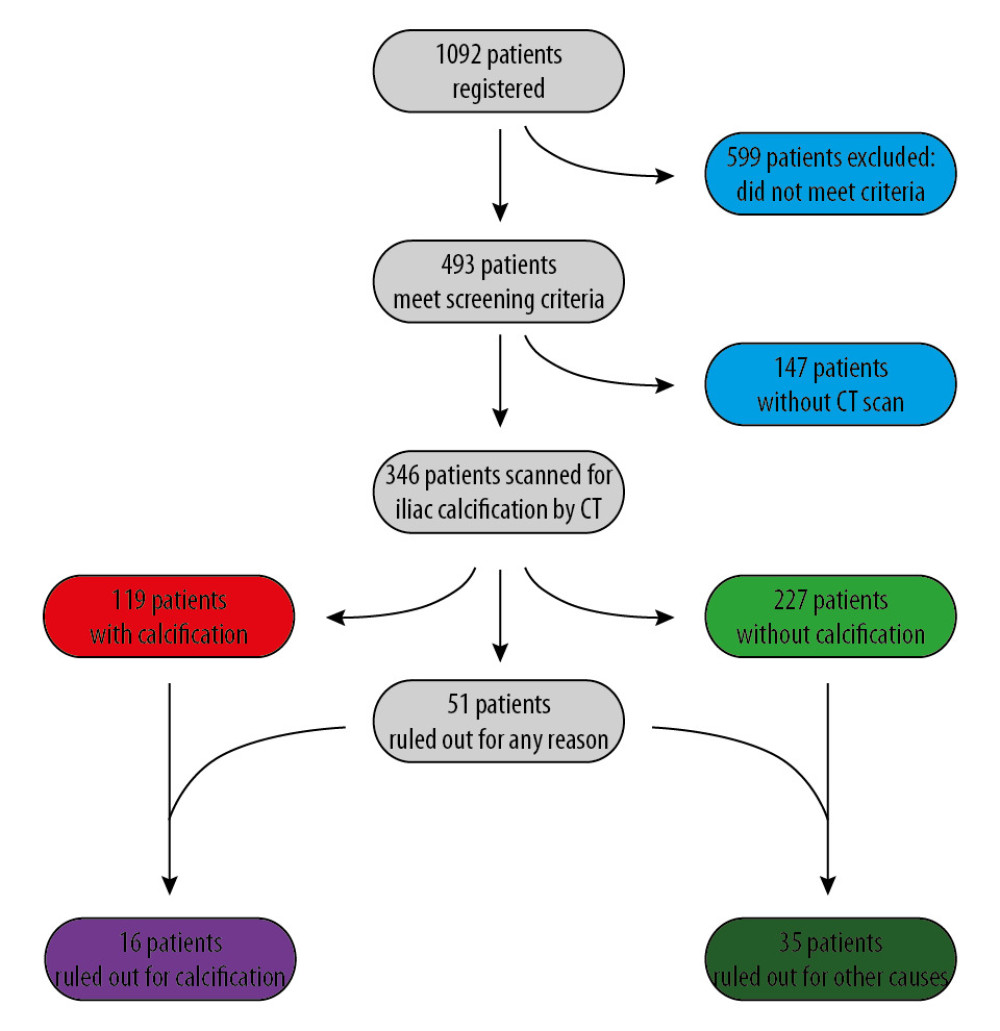 Figure 1. Study population, exclusions, outcomes of CT scanning, and candidate acceptance.
Figure 1. Study population, exclusions, outcomes of CT scanning, and candidate acceptance.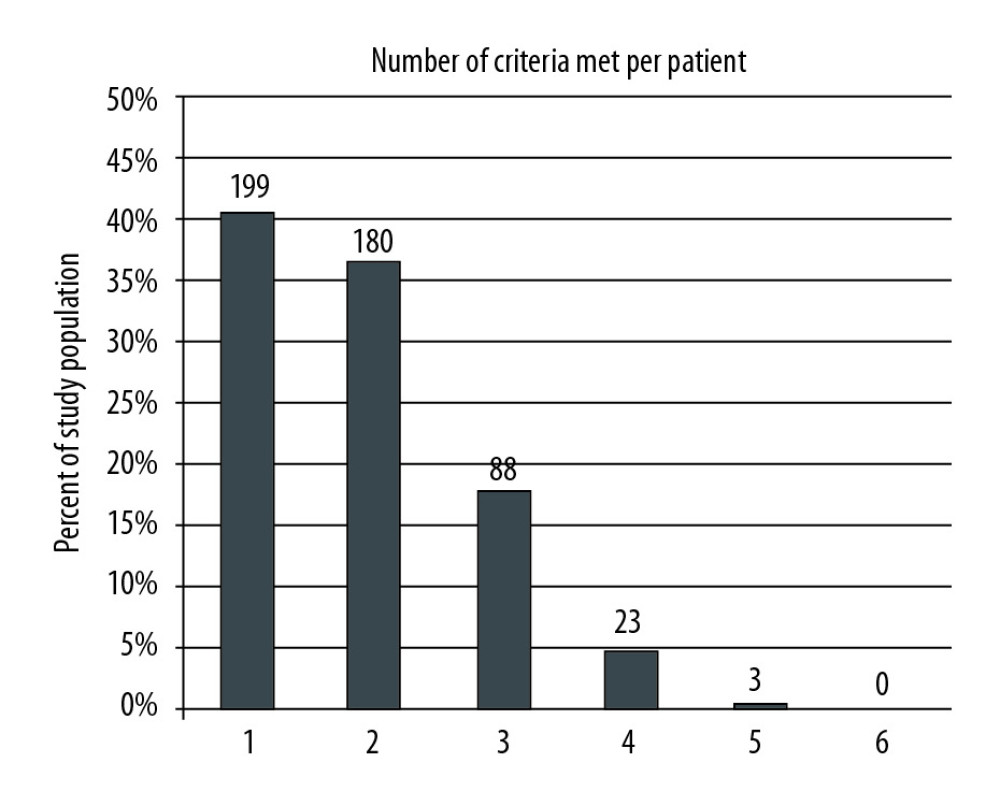 Figure 2. The patient cohort was analyzed to determine how many of the 6 screening criteria each patient met. The number of patients and percentage of the entire cohort meeting 1 through 6 of the criteria is shown. The majority of patients met 1 or 2 of the criteria.
Figure 2. The patient cohort was analyzed to determine how many of the 6 screening criteria each patient met. The number of patients and percentage of the entire cohort meeting 1 through 6 of the criteria is shown. The majority of patients met 1 or 2 of the criteria.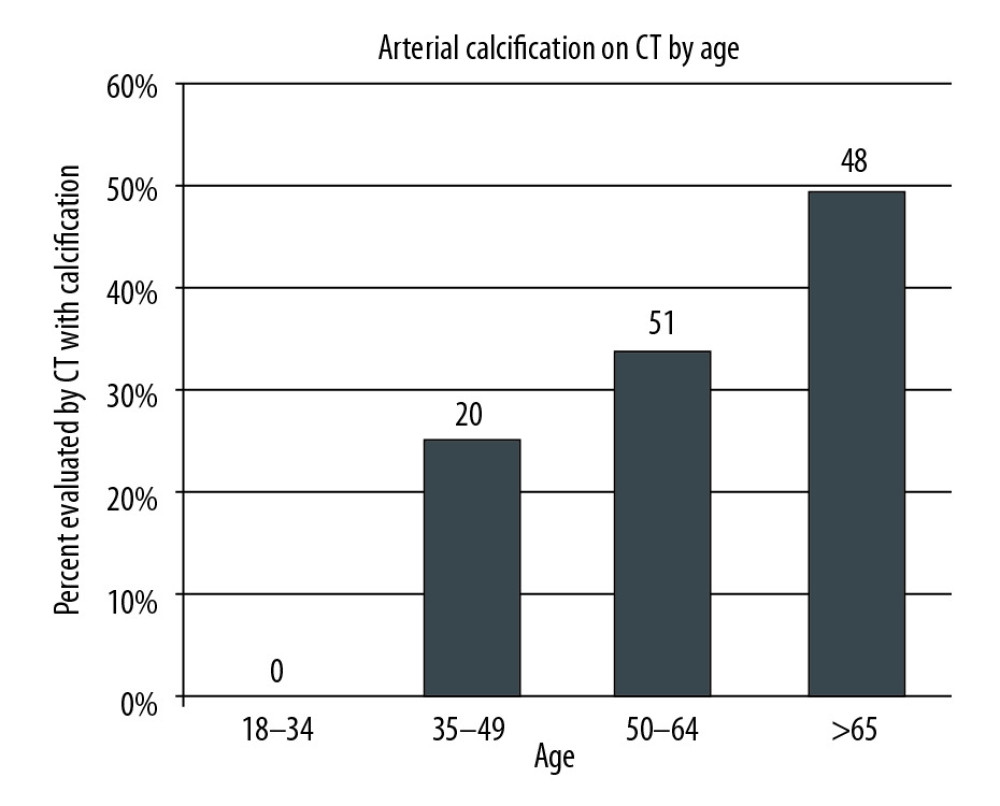 Figure 3. Age distribution of patients that were found to have iliac arterial calcification on CT scan.
Figure 3. Age distribution of patients that were found to have iliac arterial calcification on CT scan.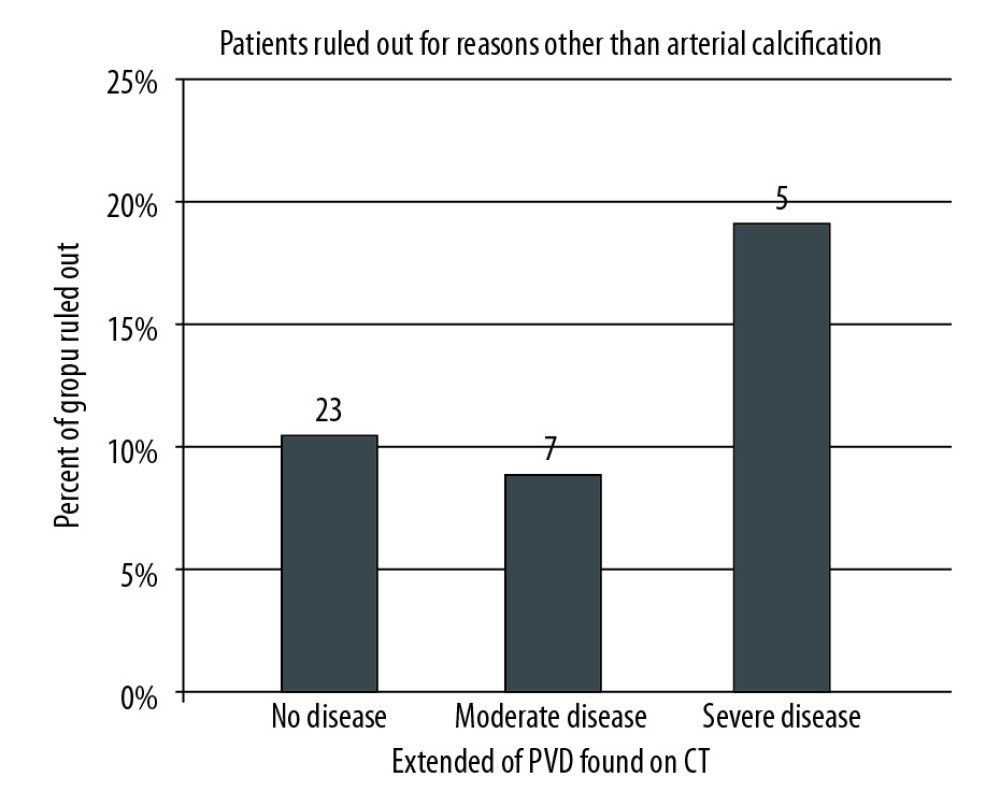 Figure 4. Patients evaluated with CT scan were categorized by the extent of iliac arterial calcification found on CT: no, moderate, or severe disease. Each group was further analyzed to determine the percentage of patients who were ruled out for other or additional reasons. Patients who were ruled out exclusively on the basis of arterial calcification were excluded from this analysis.
Figure 4. Patients evaluated with CT scan were categorized by the extent of iliac arterial calcification found on CT: no, moderate, or severe disease. Each group was further analyzed to determine the percentage of patients who were ruled out for other or additional reasons. Patients who were ruled out exclusively on the basis of arterial calcification were excluded from this analysis. Tables
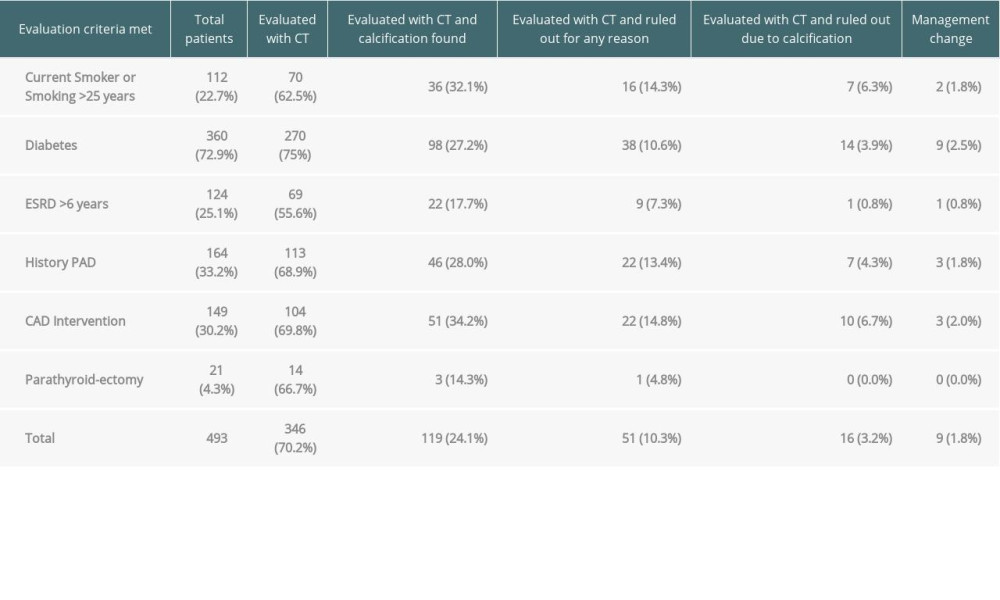 Table 1. Analysis of evaluated patients based on six screening criteria.
Table 1. Analysis of evaluated patients based on six screening criteria.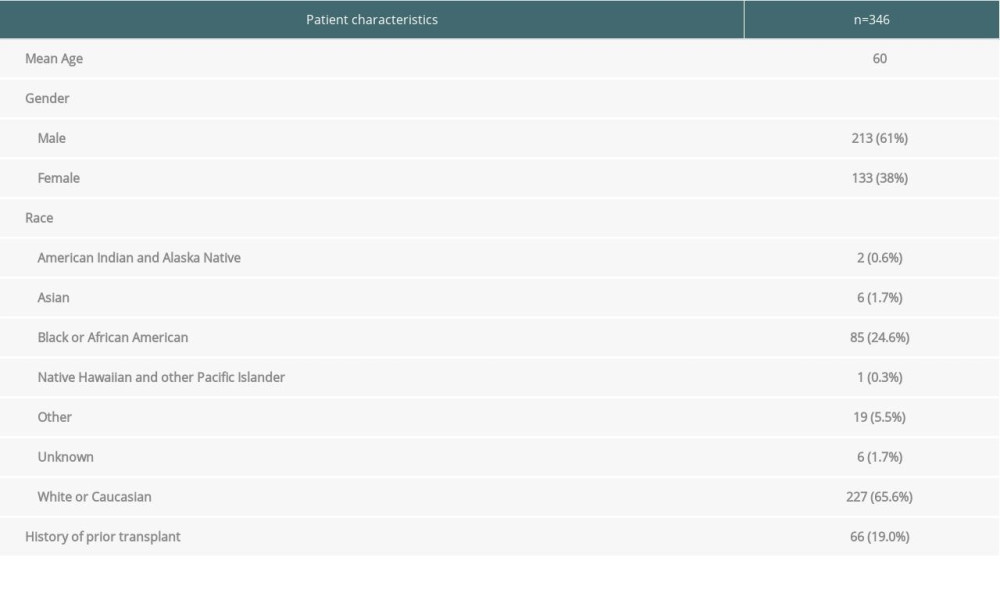 Table 2. Patient characteristics.
Table 2. Patient characteristics.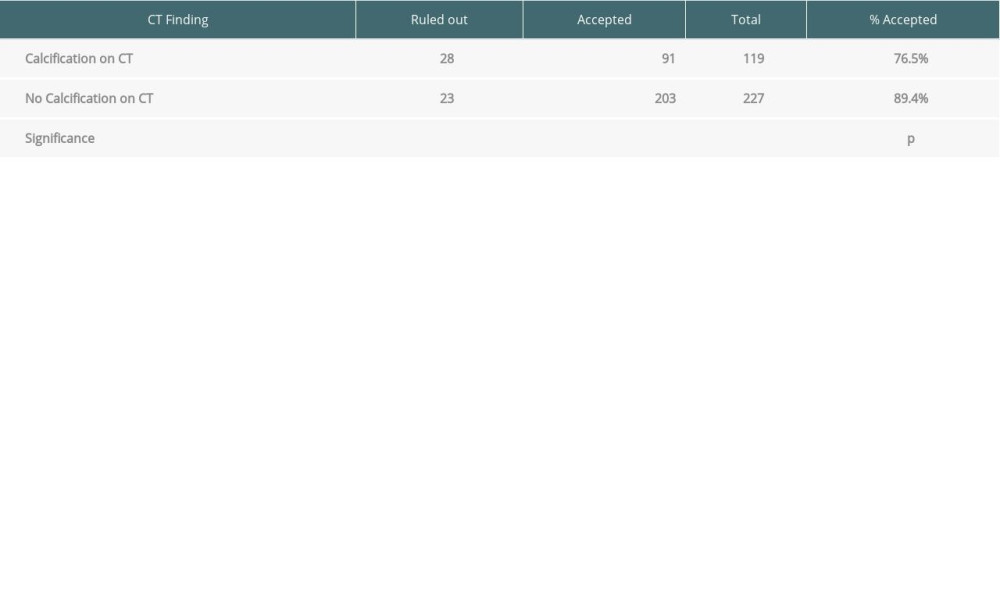 Table 3. Impact of finding iliac arterial calcification on CT scan on listing decision.
Table 3. Impact of finding iliac arterial calcification on CT scan on listing decision.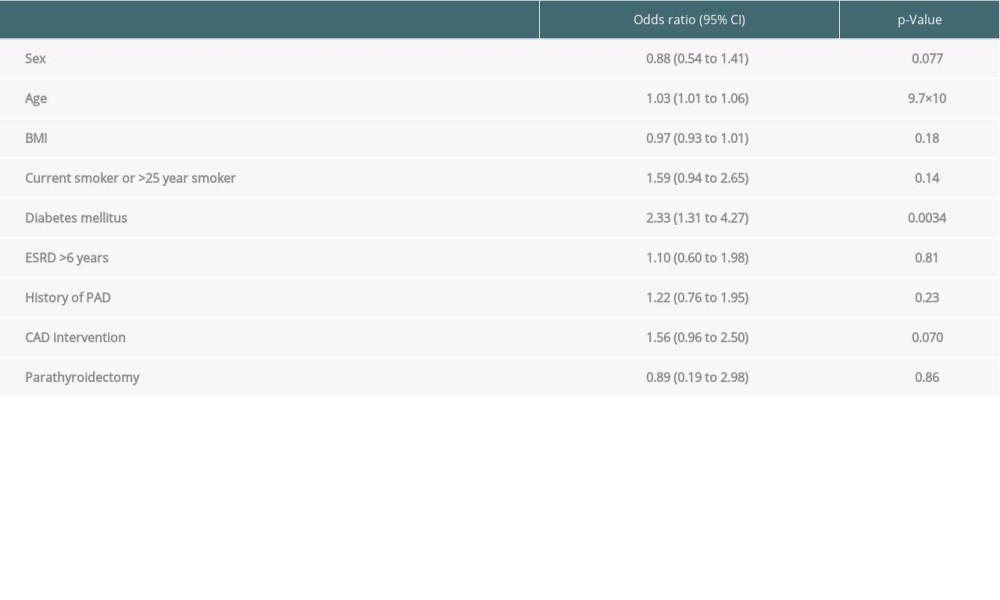 Table 4. Multivariate regression analysis.
Table 4. Multivariate regression analysis.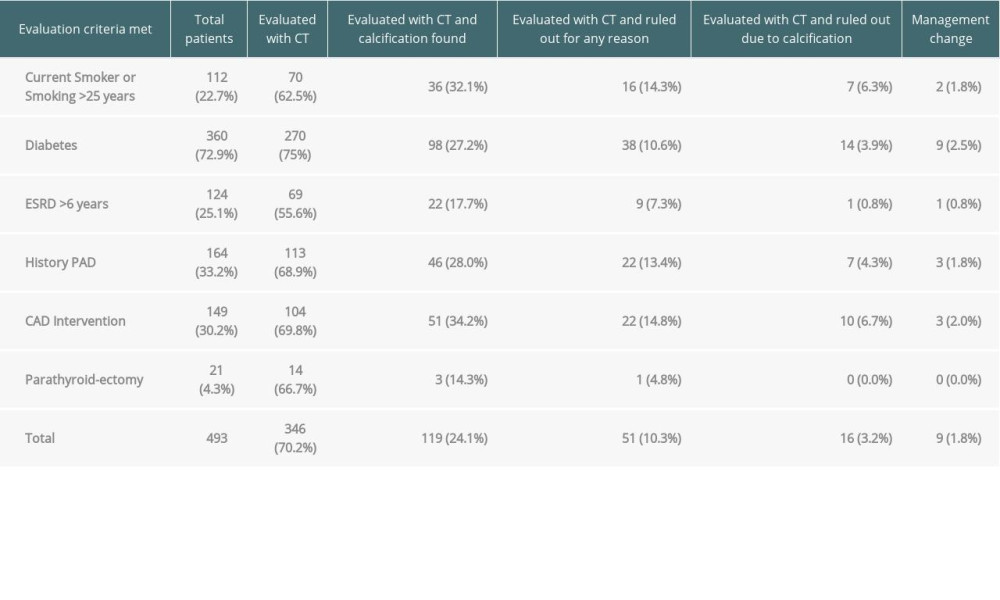 Table 1. Analysis of evaluated patients based on six screening criteria.
Table 1. Analysis of evaluated patients based on six screening criteria.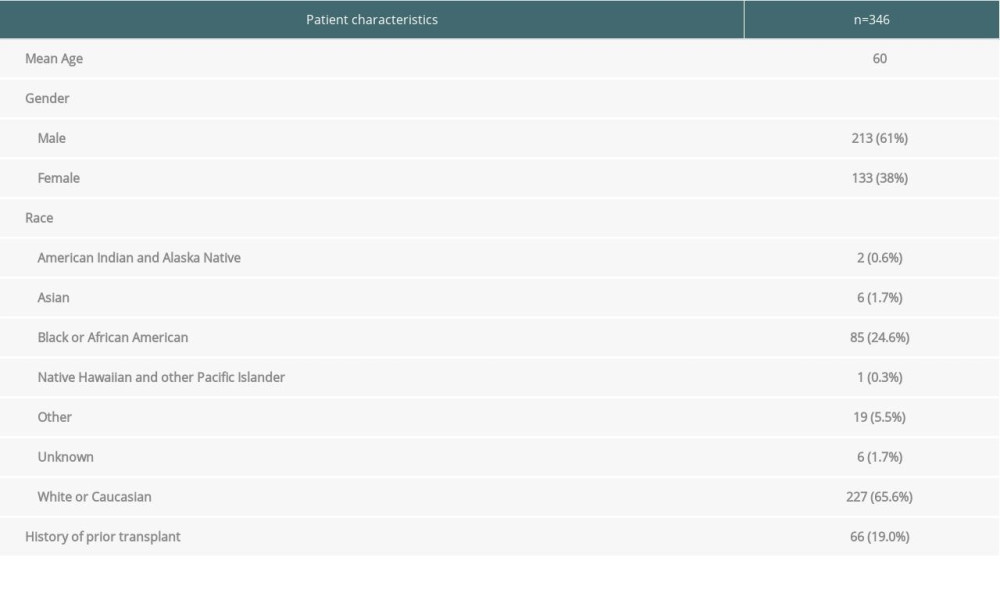 Table 2. Patient characteristics.
Table 2. Patient characteristics.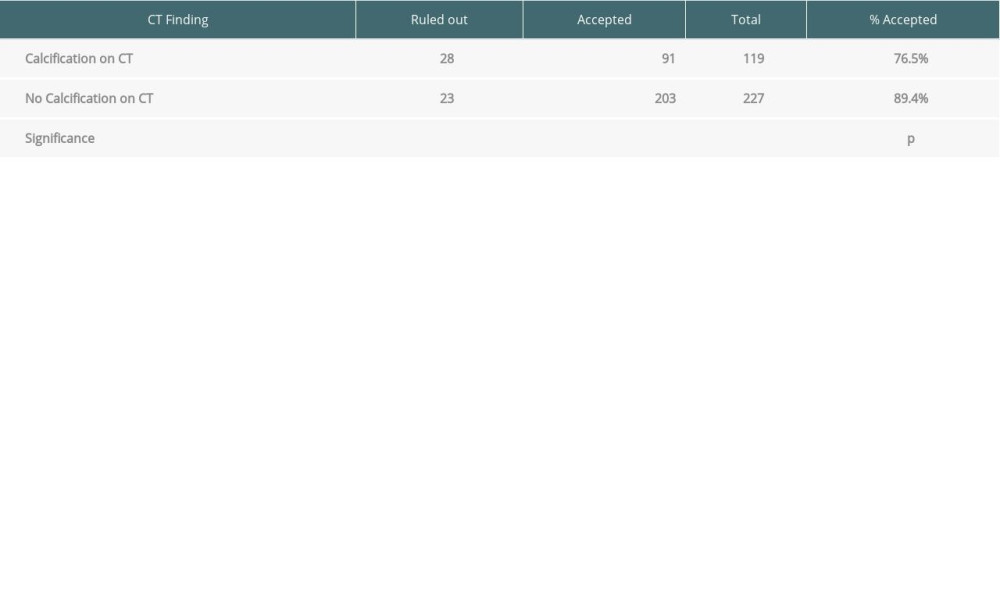 Table 3. Impact of finding iliac arterial calcification on CT scan on listing decision.
Table 3. Impact of finding iliac arterial calcification on CT scan on listing decision.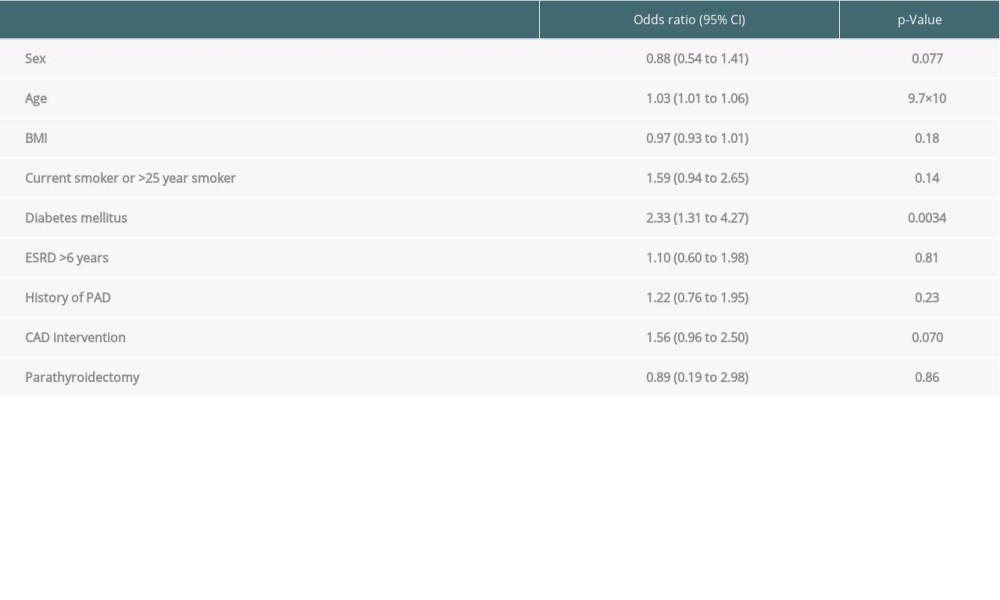 Table 4. Multivariate regression analysis.
Table 4. Multivariate regression analysis. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








