26 January 2021: Original Paper
Number of Bronchoscopic Interventions in Lung Transplant Recipients Correlates with Respiratory Function Assessed by Pulmonary Function Tests
Mirosław Nęcki12ACEF, Magdalena Latos12BCEF*, Maciej Urlik12BD, Remigiusz Antończyk12BC, Martyna Gawęda12BEF, Anastazja Pandel12BCD, Tomasz Stącel12AF, Piotr Przybyłowski3A, Marian Zembala12F, Marek Ochman12AFDOI: 10.12659/AOT.927025
Ann Transplant 2021; 26:e927025
Abstract
BACKGROUND: Lung transplant recipients may suffer from airway stenosis (AS). The aim of this study was to assess whether pulmonary function (as measured by spirometry and a 6-minute walk test [6MWT]) in patients with AS treated consistently with bronchoscopic interventions (BIs) was comparable to that in their AS-free counterparts at the 1-year follow-up visit.
MATERIAL AND METHODS: Fifty patients who underwent primary double-lung transplantation between January 2015 and March 2019 at a single center (23 who received BIs and 27 who did not) were enrolled in this retrospective study. Graft function was assessed with spirometry, based on forced expiratory volume (FEV₁) and forced vital capacity (FVC), both measured in liters (L) and percentages (%), and the Tiffeneau-Pinelli index (FEV₁/FVC), and a 6MWT and parameters such as oxygen saturation measured before and after the test.
RESULTS: Patients in need of BIs had significantly lower FEV₁% compared with individuals who did not receive BIs during their first post-transplant year. Airway obstruction was present in 22% of patients who did not receive BIs and 65.23% of those who did receive the interventions. There were statistically significant, strong, negative correlations pertaining to the number of balloon BIs and 1-year FEV₁% (rs=0.67) as well as the number of balloon BIs and 1-year FEV₁/FVC (rs=0.72). A statistically significant, strong, negative correlation (rs=0.75) was found between the number of balloon bronchoplasty treatments and oxygen saturation after the 6WMT.
CONCLUSIONS: Despite receiving BIs, patients who experience bronchial stenosis may not obtain the expected ventilatory improvement at their 1-year follow-up visit. Their AS may recur or persist despite use of various procedures. Further study in that regard is required.
Keywords: airway management, Bronchoscopy, Lung Transplantation, Respiratory Function Tests, Forced Expiratory Volume, Lung, transplant recipients
Background
Lung transplantation is the ultimate treatment for patients with end-stage lung disease. The survival rate after the procedure is good, with 50% of patients living 7.8 years after double-lung transplantation [1]. The procedure also is associated with improved pulmonary function and exercise capacity [2]. However, a significant number of double-lung recipients do not achieve 80% of predicted forced vital capacity (FVC) during their first post-transplant year [3]. In some cases, the finding can be explained by a ventilatory defect caused by airway complications located in bronchial anastomoses [4,5]. Prevalence is reported to range from 10% to 33%, but most experts agree that such complications occur in approximately 15% of lung transplant recipients [4,6,7]. Many factors, such as graft ischemic time and pretransplant microbiological colonization, can contribute to development of airway stenosis (AS) [5,6]. During the post-transplant period, patients may experience airway complications such as bronchial stenosis, exophytic necrotic tissue, and bronchomalacia [5]. Bronchoscopic interventions (BIs) available include balloon bronchoplasty, cryotherapy, argon plasma coagulation, and laser therapy; in some cases, airway stenting is a last resort [4]. Even though AS does not influence survival in graft recipients, it can cause persistent airflow limitation despite frequent use of BIs [8]. Questions remain about whether BIs used to treat AS can improve a patient’s ventilation permanently and whether these measures can improve spirometry results such that they are comparable to those in lung recipients who do not have AS. The aim of the present study was to assess whether pulmonary function (as measured by spirometry and a 6-minute walk test [6MWT]) in patients with AS treated consistently with BIs was comparable to that in their AS-free counterparts at the 1-year follow-up visit.
Material and Methods
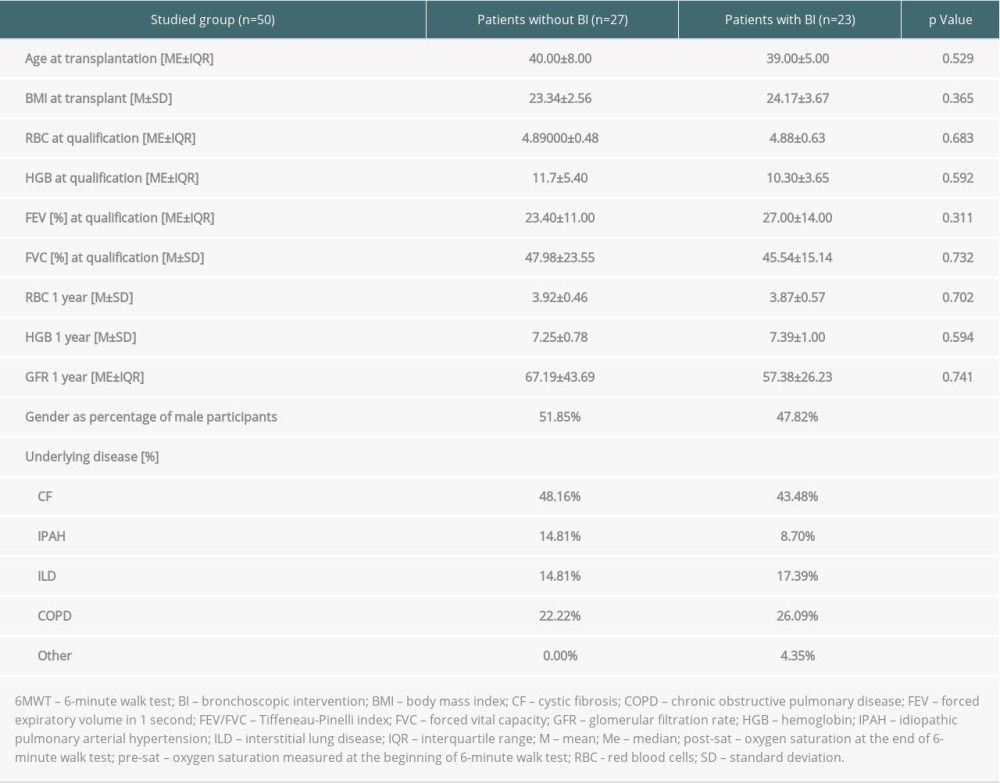
This retrospective study included 50 patients who underwent primary double-lung transplantation between January 2015 and March 2019 in our facility and had reached at least 1-year follow-up. The inclusion criteria were transplantation at age 15 years or older and absence during the study period of conditions or related procedures that would influence lung function, such as acid reflux, fundoplication surgery, and musculoskeletal disorders. Exclusion criteria were single-lung transplantation, retransplantation during the follow-up period, and existence of conditions such as a significant aortic aneurysm that would prevent performance of pulmonary function testing during the study follow-up. Detailed characteristics of the patients are listed in Table 1.
In the present study, graft function was assessed with spirometry and the Tiffeneau-Pinelli index and measurement of oxygen saturation before and after a 6MWT. Spirometry consisted of measurement of forced expiratory volume (FEV1) and forced vital capacity (FVC), both in liters (L) and percentages (%). The Tiffeneau-Pinelli index is FEV1/FVC. All of the tests were performed on the first day of patient admission for the 1-year follow-up visit after lung transplantation. Any BIs were performed after the testing because the aim of the study was to assess lung function 1 year after lung transplantation. Airway obstruction was defined as FEV1/FVC <70%. Results obtained from 6MWTs that were terminated for non-pulmonary reasons, such as a significant increase in blood pressure or active musculoskeletal injury of the lower limbs, were excluded from the study.
The primary endpoint of the study was to assess whether there was a difference in pulmonary function in patients who required BIs. The study group was divided into 2 groups: patients who did not undergo BI and those who had ≥1 BI during the first year after transplantation. BI was performed mainly by means of balloon dilation, but cryotherapy, laser therapy, and argon plasma coagulation also were used. Hypertrophic stenoses of the bronchial anastomoses in the course of complicated healing were the main reason for the aforementioned treatment. None of the patients experienced bronchial dehiscence.
Statistical analysis was carried out using TIBCO Statistica 13.30 software, including assessment of basic statistics and Shapiro-Wilk tests. A
Results
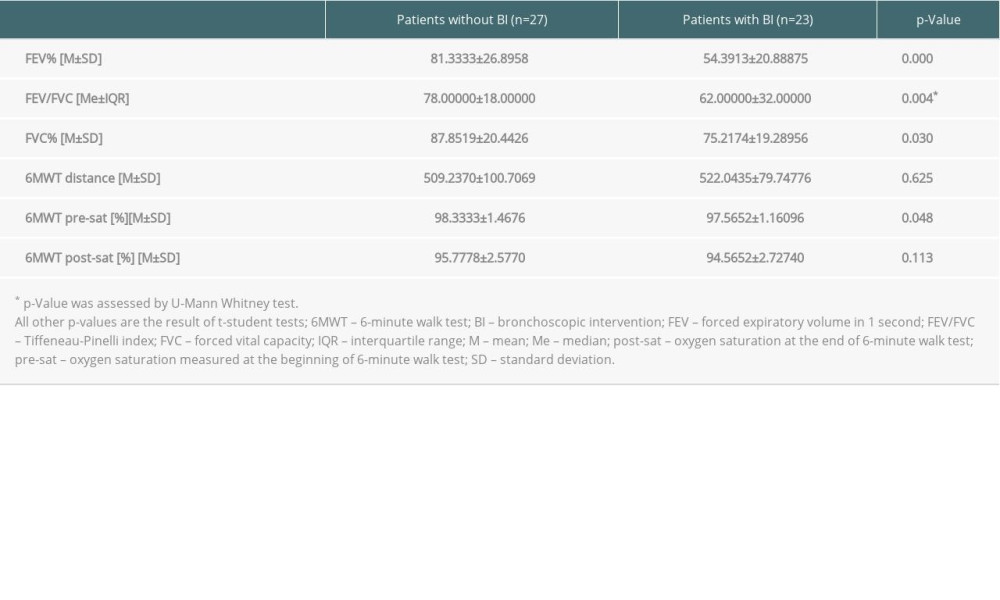
Twenty-three of 50 patients assessed during 1-year follow-up required ≥1 BI that involved, at a minimum, balloon bronchoplasty. The mean number of BIs in the study population was 6.78±5.89 (minimum 1, maximum 19). The primary endpoint of the study was to assess whether patients who underwent ≥1 BI during the first year had worse results on pulmonary function tests performed during the routine check-up visit 1 year after lung transplantation. Spirometry parameters such as FEV1, FVC, and the Tiffeneau-Pinelli index were evaluated. Detailed results of testing are shown in Table 2. Patients who underwent BIs because of significant AS had significantly lower FEV1% compared with those without BI during their first post-transplant year. Similar results were demonstrated for mean FVC%. Airway obstruction was present in 22% of patients without BI as well as 65.23% of those with a history of BI. Median values for the Tiffeneau-Pinelli index differed significantly in patients, depending on their BI status, as shown in Table 2. During every follow-up visit, our patients perform the 6MWT. There was no statistically significant difference between the groups in distance achieved on this test. However, oxygen saturation measured before the test was notably lower in the patients who had undergone ≥1 BI during their first post-transplant year. A comparison of the 6MWT results is shown in Table 2.
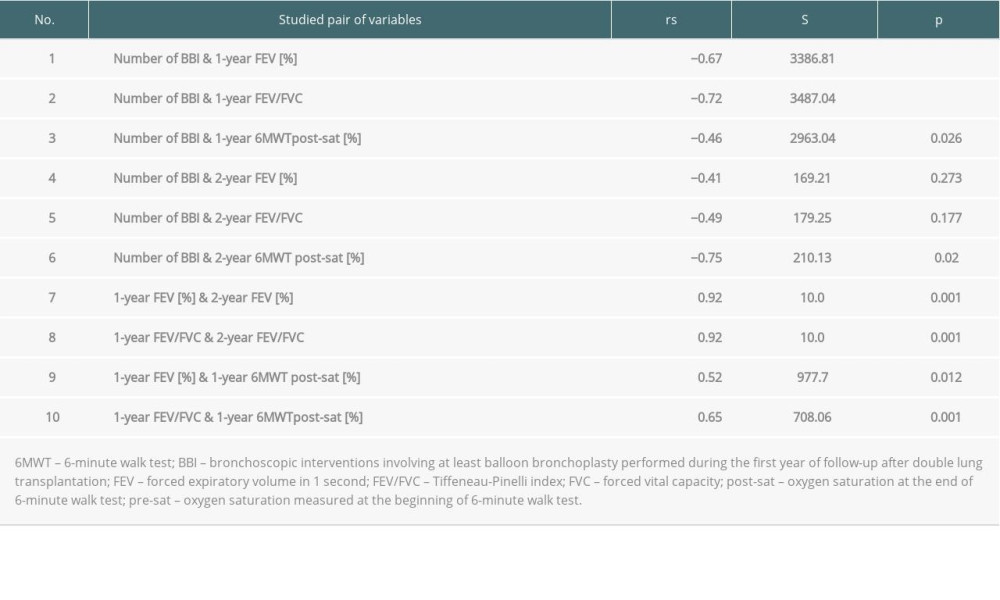
Further investigations were performed to establish whether there was a connection between BI and results of pulmonary function tests. Our analyses were based on a Spearman rank correlation coefficient, as shown in Table 3. The impact on spirometry parameters of the number of BIs involving at least balloon B was established. There were statistically significant, strong, negative correlations between the number of balloon BIs and 1-year FEV1% (rs=0.67) and the number of balloon BIs and 1-year FEV1/FVC (rs=0.72). Balloon BI did not have an effect on 1-year FVC%.
No correlation was found between the number of balloon BIs and distance on the 6MWT. However, the aforementioned analyses showed that there was a statistically significant, moderate, negative correlation (rs=0.46) between balloon BI and oxygen saturation measured at the end of the 6MWT (6MWT post-sat). Spirometry parameters such as FEV1% and FEV1/FVC also had a statistically significant, strong, positive correlation with 6MWT post-sat.
The data gathered allowed the researchers to assess whether balloon BI would also influence spirometry results at 2-year follow-up; the differences in those outcomes were not statistically significant. Nevertheless, we found that the more balloon BIs patients undergo, the worse their 6MWT post-sat may be at the 2-year check-up visit (statistically significant, strong, negative correlation of rs=0.75).
Our clinical observations led us to statistically test whether there was a chance of improvement in the pulmonary function tests over time. We found statistically significant, very strong, positive correlations between FEV1% obtained at 1 and 2 years (rs=0.92). This means that patients who underwent BI during the first year will most likely have similar FEV1% in the first and second years after transplant. We made the same observation in regard to FEV1/FVC (rs=0.92).
Discussion
Spirometry is considered to be the cornerstone of graft function monitoring [3]. Our study revealed that in patients who required ≥1 BI during their first post-transplant year, spirometry parameters were statistically significantly lower than in patients who did not need such bronchoscopic treatment. A similar finding was reported by Mazzetta et al. [8], who found that patients with central AS so severe it required BI had lower FEV1 (L) and FEV1/FVC at 18-month follow-up (81±13% versus 61±14%,
Our study assessed patients during the first visit after reaching 1-year follow-up. We also reported a statistically significant difference between our study groups in FEV1 (%) between our study groups (81±27% versus 54±21%,
In our study, patients who required BI reported significantly lower FVC% than their BI-free counterparts (75±19% versus 88±20%, P=0.03). Thirty percent of BI-free patients did not achieve FVC ≥80%, compared with 52% of those who required BI. Our study also indicates that the more balloon bronchoplasty procedures patients require during the first post-transplant year, the worse spirometry parameters they may present at 1- and 2-year follow-up because the aforementioned statistical analyses showed a strong, negative correlation between BI and those parameters. As described by Sinha, even though balloon bronchoplasty alone provides intermediate improvement, its effects are not long-lasting. In some cases, AS dilatation may be needed every 2 to 4 weeks [9]. It seems that BI other than stenting is only a palliative measure for maintaining airway patency. As reported by Shofer et al., only 37% of patients will have resolution of bronchial complications with bronchoplasty alone, and, ultimately, more than 50% of those individuals will require airway stenting [7]. Improvement in ventilation as assessed by spirometry has been reported after stent placement [10]. However, this therapeutic method is not free from adverse effects. Stent placement reportedly is associated with mucus plugging, ingrowth of granulation tissue, and microbiological colonization and harm when a stent migrates [9]. That is why AS stenting should be a last-resort treatment [11].
To the best of our knowledge, no reports exist about the influence of AS and BI on exercise capacity assessed by the 6MWT. It is important to note that the worse a patient’s FEV1% at 1-year follow-up, the worse his or her oxygen saturation after the 6MWT is likely to be. This finding may have clinical implications because it indicates that unsatisfactory ventilation is connected with oxygen deficit during exercise. The distance on the 6MWT did not differ between our study groups.
Because every bronchoscopic technique has adverse effects, such procedures should only be performed in carefully selected patients [9].
Conclusions
BIs without stenting may result in temporary improvement in individuals who have undergone primary double-lung transplantation. Despite use of these therapies, however, patients who experience bronchial stenosis may not obtain expected long-term improvement in ventilatory parameters at the 1-year follow-up visit. It is notable that CAS can recur or persist even when various BIs are used. The present study also suggests that unsatisfactory ventilation may be connected with oxygen deficit during exercise. The number of balloon bronchoplasty procedures a patient has undergone may be associated with worse results obtained during spirometry and on the 6MWT. Further study is required.
References
1. Chambers D, Cherikh W, Harhay M, The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-sixth adult lung and heart-lung transplantation Report — 2019; Focus theme: Donor and recipient size match: J Heart Lung Transplant, 2019; 38(10); 1042-55
2. Bartels M, Armstrong H, Gerardo R, Evaluation of pulmonary function and exercise performance by cardiopulmonary exercise testing before and after lung transplantation: Chest, 2011; 140(6); 1604-11
3. Mohanka MR, Kanade R, Garcia H, Significance of best spirometry in the first year after bilateral lung transplantation: Association with 3-year outcomes: Transplantation, 2020; 104(8); 1712-19
4. Varela A, Hoyos L, Romero A, Management of bronchial complications after lung transplantation and sequelae: Thorac Surg Clin, 2018; 28(3); 365-75
5. Mahajan AK, Folch E, Khandhar SJ, The diagnosis and management of airway complications following lung transplantation: Chest, 2017; 152(3); 627-38
6. Yserbyt J, Dooms C, Vos R, Anastomotic airway complications after lung transplantation: Risk factors, treatment modalities and outcome – a single-centre experience: Eur J Cardiothoracic Surg, 2016; 49(1); e1-8
7. Shofer SL, Wahidi MM, Davis WA, Significance of and risk factors for the development of central airway stenosis after lung transplantation: Am J Tranplant, 2013; 13(2); 383-89
8. Mazzetta A, Porzio M, Riou M, Patients treated for central airway stenosis after lung transplantation have persistent airflow limitation: Ann Transplant, 2019; 24; 84-92
9. Sinha N, Transplant pulmonary interventions: Translating lung transplant interventions to nontransplant patients: Methodist Debakey Cardiovasc J, 2016; 12(4); 18-20
10. Chhajed PN, Malouf MA, Tamm M, Interventional bronchoscopy for the management of airway complications following lung transplantation: Chest, 2001; 120(6); 1894-99
11. Frye L, Machuzak M, Airway Complications after lung transplantation: Clin Chest Med, 2017; 38(4); 693-706
In Press
15 Mar 2024 : Review article
Approaches and Challenges in the Current Management of Cytomegalovirus in Transplant Recipients: Highlighti...Ann Transplant In Press; DOI: 10.12659/AOT.941185
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860