08 February 2022: Original Paper
Impact of Thyroid Incidentaloma on Liver Transplant: A Study of 1010 Recipients at a Single Center
Yi-Chia ChanDOI: 10.12659/AOT.934988
Ann Transplant 2022; 27:e934988
Abstract
BACKGROUND: Thyroid incidentalomas are typically nonpalpable thyroid nodules discovered during radiographic evaluation for a non-thyroid issue. Thyroid incidentalomas visualized by computed tomography (CT) and ¹⁸F-flurodeoxyglucose (FDG) positron emission tomography (PET) before living donor liver transplantation (LDLT) are rare. The aim of the study was to analyze the clinical impact of thyroid incidentalomas discovered prior to transplantation.
MATERIAL AND METHODS: This retrospective study recruited 1010 patients undergoing LDLT between 2010 and 2019. CT was performed on each patient, whereas PET was performed on randomized patients (n=498).
RESULTS: The prevalence and malignant risk of thyroid incidentaloma on CT was 2.3% (23/1010) and 13.0% (3/23), respectively. The prevalence of thyroid incidentaloma on PET was 3.0% (15/498). Approximately half of the FDG uptake on PET was diffuse uptake (n=7), whereas the other half was focal uptake (n=8). The malignant risk of PET incidentaloma with focal FDG uptake was 37.5% (3/8). Four asymptomatic thyroid cancers were identified incidentally. After total thyroidectomy followed by LDLT, these patients maintained cancer-free status.
CONCLUSIONS: Thyroid incidentalomas occurred at a rate of 2-3% in LDLT candidates. The malignant risk was 13.0% on CT incidentaloma, and 37.5% on PET incidentaloma with focal FDG uptake. Curative treatment of incidental thyroid cancer followed by LDLT without delay can achieve a favorable prognosis.
Keywords: Incidental Findings, Liver Transplantation, Thyroid Diseases, Fluorodeoxyglucose F18, Humans, Living Donors, Positron Emission Tomography Computed Tomography, Thyroid Neoplasms, Tomography, X-Ray Computed
Background
The prevalence of impalpable thyroid nodules in the general population may be up to 50% on autopsy, but most of these nodules are asymptomatic [1]. With advancement in imaging technologies and increased utility of imaging modalities, incidental thyroid nodules are being increasingly identified. Several studies have investigated the clinical impact of thyroid incidentalomas noted on computerized tomography (CT), magnetic resonance imaging, ultrasound (US), and 18F-flurodeoxyglucose (FDG) positron emission tomography (PET) in the general population for cancer screening or in patients with documented malignancy unrelated to the thyroid [2–4].
Liver cirrhosis is a leading cause of mortality and morbidity, with mortality rates rising globally between 1990 and 2017 [5]. Liver transplantation (LT) is the most effective surgical treatment for liver cirrhosis. However, several studies indicated that LT recipients had greater risks of de novo or recurrent cancers during follow-up [6–8]. The etiology may come from the immunosuppressive therapy, including attenuation of cytotoxic T-cell and natural killer cell function, as well as the disturbance of humoral interaction with macrophages [9,10]. Additionally, reports from animal studies demonstrated that calcineurin inhibitors (CNIs), one of the most common immunosuppressive drugs, have carcinogenic effect, which may be caused by activation of Ras pathway, induction of tumor growth, and disruption of angiogenesis and apoptosis [11–13]. Therefore, surveying of extrahepatic malignancy before LT and curative treatment of pre-existing malignancy is recommended, with sufficient time for observation of recurrence or metastasis [14].
When chest CT or 18F-FDG PET were arranged to survey malignancy [15,16], thyroid mass might be identified incidentally. Based on the current recommendations from American Thyroid Association (ATA), fine needle aspiration (FNA) was probably perceived to define the benign or malignant nature of the thyroid incidentaloma [17,18]. Once the patient was diagnosed of thyroid cancer, a decision had to be reached as to whether LT surgery should be delayed [14].
The aim of this study was to describe the prevalence and malignant risk of thyroid incidentaloma discovered on CT or 18F-FDG PET in a large series of patients with liver cirrhosis or hepatocellular carcinoma (HCC) scheduled for upcoming LDLT. This study also aimed to evaluate the impact of untreated thyroid cancer discovered prior to LDLT on the clinical course and long-term outcome.
Material and Methods
STUDY POPULATION AND DESIGN:
The study sample comprised 1010 adults (all >20 years old) who underwent LDLT at Kaohsiung Chang Gung Memorial Hospital in Taiwan between January 2010 and December 2019. We maintained a longitudinal database of recipients and recorded all demographic, pre-operative, peri-operative, pathological, and follow-up information. All patients were followed up at our outpatient clinic every 3–6 months, with the observation period terminating in July 2021. The study was approved by the Institutional Review Board (IRB no. 202101208B0), and the need to obtain informed consent from patients was waived due to the study’s retrospective design.
Patients were excluded if they had a previous thyroid disease or symptomatic thyroid mass. Two patients with underlying Graves’ disease and 1 patient with benign nodular goiter post-lobectomy were excluded from the study.
The pre-operative assessment of LT candidates included screening for cardiovascular risk, psychological examination, and radiological assessment of the hepatic vasculo-biliary anatomy. The 64-raw multidetector chest CT (Aquilion 64; Toshiba Medical System; Japan) with both lung (window width 1500 H; window level −500 H) and soft tissue (window width 350 H, window level 50 H) settings was also performed routinely to survey lung lesions [15], and interpreted by the radiologists. FDG-PET scan (Discovery ST; GE Healthcare; USA), reviewed by the nuclear radiologists, was performed to exclude the possibility of distant HCC metastasis or extrahepatic malignancy [16], both of which are contraindication of LT [14]. Due to the prohibitively expensive cost of PET scan, it was performed on half of the sample participants in a randomized manner (n=498, 49%). For each patient with incidental thyroid mass on chest CT or PET scan, serum thyroid-stimulating hormone (TSH), thyroid hormone, and thyroid antibodies were measured, and thyroid US were performed.
Thyroid US (LOGIQ S8; GE Healthcare; USA) was performed by endocrinologists or general surgeons. FNA cytology with a 21-gauge needle was indicated when a definite solid nodule was noticed on US, and the specimen was examined by the same groups of cytologists. FNA was performed for every solid nodule without size limitation, but FNA was not performed for pure cystic lesions. If the cytology report indicated the presence of atypical cells, follicular neoplasm, and suspicious or confirmed malignancy, diagnostic thyroidectomy was recommended and performed prior to LT to confirm the diagnosis and cancer staging.
DEFINITIONS:
Excluding primary biliary cholangitis and primary sclerosis cholangitis, the diagnosis of autoimmune hepatitis was made based on the serological and/or histopathologic reports from the explants or on revised International Autoimmune Hepatitis Group scoring systems [19]. Diffuse uptake on PET scan was defined as FDG uptake over the entire thyroid gland, whereas focal uptake was defined as localized FDG uptake in the thyroid. Regions of interests were drawn for quantification FDG uptake on the visible lesions with increased tracer uptake, and maximum standard uptake values (SUVs) were calculated and recorded. Hypothyroidism was defined as a TSH level exceeding the reference range and a free thyroxine (FT4) level falling below the reference range, a documented history of hypothyroidism, or the use of thyroid hormone replacement therapy [20]. Autoimmune thyroiditis, also known as chronic lymphocytic or Hashimoto’s thyroiditis, was defined by the presence of specific auto-antibodies in serum, including antithyroid peroxidase antibodies (TPO Ab) and antithyroglobulin antibodies (Tg Ab), and by varying degrees of thyroid dysfunction [21,22]. Papillary thyroid cancer (PTC) was staged according to the 8th edition American Joint Committee on Cancer (AJCC) TNM system.
DATA COLLECTION:
Demographic and operative variables included age, sex, underlying etiology of liver disease, and presence of HCC. Preoperative and postoperative variables measured included body mass index (BMI) and the prevalence of hypertension (HTN) or diabetes mellitus (DM). Postoperative data included immunosuppressive therapy and outcome of thyroid cancer.
The primary outcome in this study was the incidence of thyroid incidentaloma on CT or PET in LT candidates. Secondary outcomes included the prevalence of subclinical thyroid cancer, the outcome of LT recipients with concurrent thyroid cancer, and the association with thyroiditis or hypothyroidism.
IMMUNOSUPPRESSIVE THERAPY:
All LDLT patients in the cohort received an initial standard immunosuppressive regimen comprising the CNI (tacrolimus) with mycophenolate mofetil. Target trough levels were 5–7 ng/mL for tacrolimus during the first year and 3–5 ng/mL after 1 year. Additionally, some patients were added on or converted to a mammalian target of rapamycin (mTOR) inhibitor for renal function preservation and anti-tumor effect.
STATISTICAL ANALYSIS:
Data were collected and analyzed using SPSS Statistics v.20 software (IBM corporation, Armonk, NY). Qualitative variables were expressed as frequency of events and cumulative incidence (in percentage). Quantitative variables were expressed by their median with inter quartile range (IQR). Differences between groups were compared using the exact Fisher test for 2 qualitative variables and the nonparametric Mann-Whitney U test was calculated for differences in 2 groups for quantitative variables. The Wilcoxon signed-rank test was used to compare the repeated measurements on a single sample in a nonparametric group. A
Results
THYROID INCIDENTALOMA ON CT:
The cohort comprised 286 females and 724 males, with a mean age of 54.5±14.9 years. Chest CT identified 23 cases (2.3%, 23/1010) of thyroid incidentaloma in 1010 LT candidates without known thyroid disease (Table 1). The demographics of the 2 groups (CT thyroid incidentaloma and no CT thyroid incidentaloma) were comparable. Thyroid echo was performed exclusively in each CT-discovered thyroid incidentaloma case, followed by FNA to obtain the diagnosis. FNA was abandoned in 3 cases due to pure thyroid cysts. Among the 4 patients with FNA whose result were Bethesda category III, IV, and VI, diagnostic thyroidectomy was performed. One case was diagnosed with nodular goiter after right thyroidectomy, and another 3 cases were found to be papillary thyroid cancer (Patient No. 1, 3 and 4; Table 2 and Figure 1) after bilateral total thyroidectomy. Due to the well-differentiated thyroid cancer without LN or distant metastasis, the 3 thyroid cancer patients underwent LDLT surgery in 1 week after thyroidectomy.
In addition, the tumor sizes measured by CT and US differed significantly (median size: 1.5 cm vs 1.7 cm;
THYROID INCIDENTALOMA IN PET:
The sample comprised 359 females and 139 males, with a mean age of 54.5±8.0 years. Among the 498 cases who underwent PET scan (Tables 1, 2), a total of 15 (3%, 15/498) thyroid incidentalomas were identified, including patterns of diffuse (n=7) and focal (n=8) uptakes. Although the demographics of both groups (PET thyroid incidentaloma and no PET thyroid incidentaloma) were similar, the prevalence rate of autoimmune hepatitis was higher in the group with PET thyroid incidentaloma than in the group without PET thyroid incidentaloma (6.7% vs 1.0%; P=0.049). Moreover, the pattern of diffuse FDG uptake (n=7, Figure 2) was suggestive of thyroiditis without definite mass on the CT scan and echo, and this pattern corresponded to autoimmune thyroiditis in 5 cases (71%, 5/7), according to serology test results. Four of 7 (57%) patients with diffuse FDG uptake in the thyroid had overt hypothyroidism without treatment (Table 2). For patients with focal FDG uptake in the thyroid (n=8), US and FNA were performed for each case. Three patients underwent total thyroidectomy because cytology results indicated Bethesda category ranging from 3–5, and they were postoperatively diagnosed with PTC (Patient No. 1, 2 and 4; Table 3 and Figure 1). Due to well-differentiated thyroid cancer without LN or distant metastasis, all patients underwent LDLT surgery in one week after thyroidectomy. For patients with PTC size >1 cm, radio-ablation therapy was scheduled according to ATA guidelines when the postoperative condition became stable [17], and these patients have maintained a thyroid cancer disease-free status to date. Moreover, in our analysis, the maximal value of SUV uptake was not associated with the occurrence of thyroid cancer (median SUV uptake of thyroid cancer vs benign nodule: 3.9 vs 3.7; P=0.840).
Discussion
STUDY LIMITATIONS:
This study has several limitations. First, this retrospective study was conducted at a single medical center, and postoperative prognosis may vary among different hospitals by virtue of differences in management. Second, when the material obtained by FNA was insufficient, we did not repeat the procedure and the final diagnosis of one-fourth thyroid incidentaloma cases were inconclusive. Therefore, the real prevalence of malignancy in incidental FDG uptake thyroid nodules remained undetermined. Third, thyroid echo and thyroid function was not assessed in each patient, which may underestimate the true incidence of thyroid incidentaloma and thyroid dysfunction. Fourth, the observation duration for postoperative thyroid cancer was insufficient (median: 50 months; range: 24–64 months) to determine long-term prognosis. To overcome these limitations, larger prospective, randomized controlled trials are needed.
Conclusions
Incidental thyroid mass visualized on CT or 18F-FDG PET in LT candidates was not uncommon, with a prevalence rate ranging from 2% to 3% in our study. Although diffuse FDG uptake on PET indicates benign thyroiditis, the cancer risk climbs up to 13.0% on CT and 37.5% on PET with focal FDG uptake. Due to low risk of thyroid cancer in the majority of our patients, total thyroidectomy followed by LT without delay can achieve tumor-free status with fair liver function.
Figures
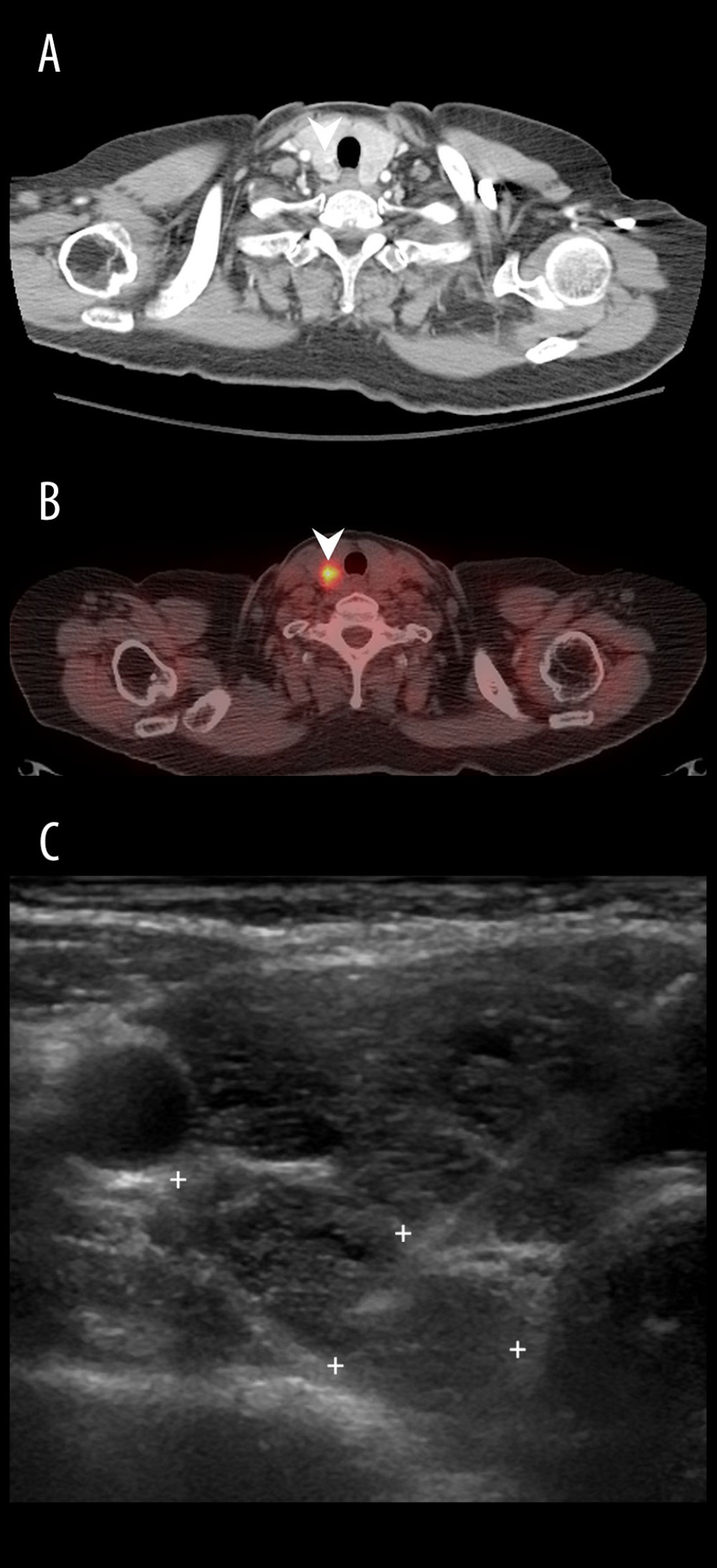 Figure 1. A 61-year-old woman (Patient No. 1) with hepatitis C-related liver cirrhosis and hepatocellular carcinoma was diagnosed with papillary carcinoma (stage I, pT1bN0M0) after total thyroidectomy. (A) Chest CT demonstrated a round isoechoic nodule with contrast-enhanced rim at right lower lobe; (B) 18F-FDG PET/CT showed a hypermetabolic tumor with SUVmax up to 6.8 at right lobe; (C) Transverse view of thyroid echo revealed an ovoid isoechoic tumor at right lower thyroid, then fine needle aspiration disclosed atypical cells.
Figure 1. A 61-year-old woman (Patient No. 1) with hepatitis C-related liver cirrhosis and hepatocellular carcinoma was diagnosed with papillary carcinoma (stage I, pT1bN0M0) after total thyroidectomy. (A) Chest CT demonstrated a round isoechoic nodule with contrast-enhanced rim at right lower lobe; (B) 18F-FDG PET/CT showed a hypermetabolic tumor with SUVmax up to 6.8 at right lobe; (C) Transverse view of thyroid echo revealed an ovoid isoechoic tumor at right lower thyroid, then fine needle aspiration disclosed atypical cells. 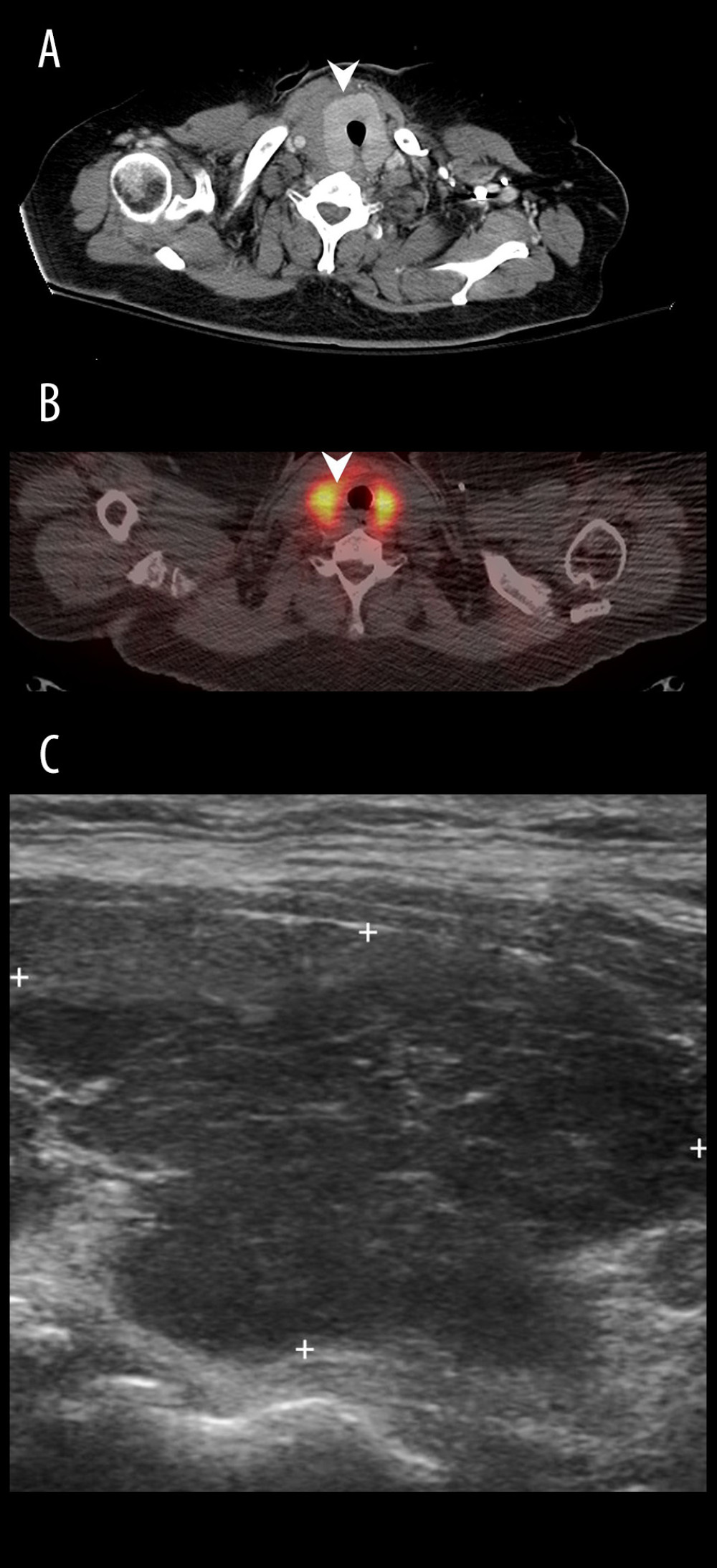 Figure 2. A 60-year-old woman with hepatitis C-related liver cirrhosis. (A) Chest CT showed an enlarged thyroid gland without mass; (B) 18F-FDG PET/CT revealed diffuse uptake over bilateral thyroid with SUVmax up to 12.8; (C) Longitudinal view of thyroid echo disclosed hypoechoic parenchyma, compatible with thyroiditis change.
Figure 2. A 60-year-old woman with hepatitis C-related liver cirrhosis. (A) Chest CT showed an enlarged thyroid gland without mass; (B) 18F-FDG PET/CT revealed diffuse uptake over bilateral thyroid with SUVmax up to 12.8; (C) Longitudinal view of thyroid echo disclosed hypoechoic parenchyma, compatible with thyroiditis change. References
1. Mortensen JD, Wolner LB, Bennett WA, Gross and microscopic findings in clinically normal thyroid glands: J Clin Endocrinol Metab, 1955; 15(10); 1270-80
2. Youserm DM, Huang T, Loevner LA, Langlotz CP, Clinical and economic impact of incidental thyroid lesions found with CT and MR: Am J Neuroradiol, 1997; 18(8); 1423-28
3. Are C, Hsu JF, Schoder H, FDG-PET detected thyroid incidentalomas: need for further investigation?: Ann Surg Oncol, 2007; 14(1); 239-47
4. Nguyen XV, Job J, Fiorillo LE, Sipos J, Thyroid incidentalomas: Practice considerations for radiologists in the age of incidental Findings: Radiol Clin North Am, 2020; 58(6); 1019-31
5. GBD 2017 Cirrhosis Collaborators, The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017: Lancet Gastroenterol Hepatol, 2020; 5(3); 245-66
6. Chandok N, Watt KD, Burden of de novo malignancy in the liver transplant recipient: Liver Transpl, 2012; 18(11); 1277-89
7. Chak E, Saab S, Risk factors and incidence of de novo malignancy in liver transplant recipients: A systematic review: Liver Int, 2010; 30(9); 1247-58
8. Penn I, Evaluation of transplant candidates with pre-existing malignancies: Ann Transplant, 1997; 2(4); 14-17
9. Penn I, The effect of immunosuppression on pre-existing cancers: Transplantation, 1993; 55(4); 742-47
10. Zitvogel L, Tesniere A, Kroemer G, Cancer despite immunosurveillance: immunoselection and immunosubversion: Nat Rev Immunol, 2006; 6(10); 715-27
11. Maluccio M, Sharma V, Lagman M, Tacrolimus enhances transforming growth factor-beta1 expression and promotes tumor progression: Transplantation, 2003; 76(3); 597-602
12. Yarosh DB, Pena AV, Nay SL, Calcineurin inhibitors decrease DNA repair and apoptosis in human keratinocytes following ultraviolet B irradiation: J Invest Dermatol, 2005; 125(5); 1020-25
13. Datta D, Contreras AG, Basu A, Calcineurin inhibitors activate the proto-oncogene Ras and promote protumorigenic signals in renal cancer cells: Cancer Res, 2009; 69(23); 8902-9
14. Martin P, DiMartini A, Feng S, Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation: Hepatology, 2014; 59(3); 1144-65
15. Wu YJ, Lin CC, Lin YH, Incidentally small pulmonary nodule in candidates for living donor liver transplantation: Ann Transplant, 2015; 20; 734-40
16. Schöder H, Gönen M, Screening for cancer with PET and PET/CT: Potential and limitations: J Nucl Med, 2007; 48(Suppl 1); 4S-18S
17. Haugen BR, Alexander EK, Bible KC, 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer: Thyroid, 2016; 26(1); 1-133
18. Ammendola S, Girolami I, Bovo C, Thyroid fine-needle aspiration cytology: Focusing on adherence to guidelines and hospital organization: Am J Case Rep, 2020; 21; e920933
19. Alvarez F, Berg PA, Bianchi FB, International Autoimmune Hepatitis Group Report: Review of criteria for diagnosis of autoimmune hepatitis: J Hepatol, 1999; 31(5); 929-38
20. Zhang N, Jin W, Zhou S, Hypothyroidism is associated with worse outcomes of hepatocellular carcinoma patients after liver transplantation: Cancer Med, 2018; 7(12); 5870-78
21. Burek CL, Rose NR, Autoimmune thyroiditis and ROS: Autoimmun Rev, 2008; 7(7); 530-37
22. Dayan CM, Daniels GH, Chronic autoimmune thyroiditis: N Engl J Med, 1996; 335(2); 99-107
23. Yoon DY, Chang SK, Choi CSY, The prevalence and significance of incidental thyroid nodules identified on computed tomography: J Comput Assist Tomogr, 2008; 32(5); 810-15
24. Tao W, Qingjun Z, Wei Z, Computed tomography versus ultrasound/fine needle aspiration biopsy in differential diagnosis of thyroid nodules: a retrospective analysis: Braz J Otorhinolaryngol, 2021; 87(4); 402-9
25. Bachar G, Buda I, Cohen M, Size discrepancy between sonographic and pathological evaluation of solitary papillary thyroid carcinoma: Eur J Radiol, 2013; 82(11); 1899-903
26. Kim TY, Kim WB, Ryu JS, 18F-fluorodeoxyglucose uptake in thyroid from positron emission tomogram (PET) for evaluation in cancer patients: High prevalence of malignancy in thyroid PET incidentaloma: Laryngoscope, 2005; 115(6); 1074-78
27. Chen W, Parsons M, Torigian DA, Evaluation of thyroid FDG uptake incidentally identified on FDG-PET/CT imaging: Nucl Med Commun, 2009; 30(3); 240-44
28. Chung SR, Choi YJ, Suh CH: Thyroid, 2018; 28(6); 762-68
29. Brito JP, Hay ID, Morris JC, Low risk papillary thyroid cancer: BMJ, 2014; 348; g3045
30. Eccher A, Lombardini L, Girolami I, How safe are organs from deceased donors with neoplasia? The results of the Italian Transplantation Network: J Nephrol, 2019; 32(2); 323-30
31. Eccher A, Girolami I, Marletta S, Donor-transmitted cancers in transplanted livers: Analysis of clinical outcomes: Liver Transpl, 2021; 27(1); 55-66
32. Yasuda S, Shohtsu A, Ide M, Chronic thyroiditis: diffuse uptake of FDG at PET: Radiology, 1998; 207(3); 775-78
33. Ringel MD, Management of hypothyroidism and hyperthyroidism in the Intensive Care Unit: Crit Care Clin, 2001; 17(1); 59-74
34. Salman A, Aon M, Hussein A, Impact of hypothyroidism on patients with hepatocellular carcinoma undergoing liver transplantation: Int J Gen Med, 2021; 14; 5711-18
35. Wong GW, Yeong T, Lawrence D, Concurrent extrahepatic autoimmunity in autoimmune hepatitis: implications for diagnosis, clinical course and long-term outcomes: Liver Int, 2017; 37(3); 449-57
Figures
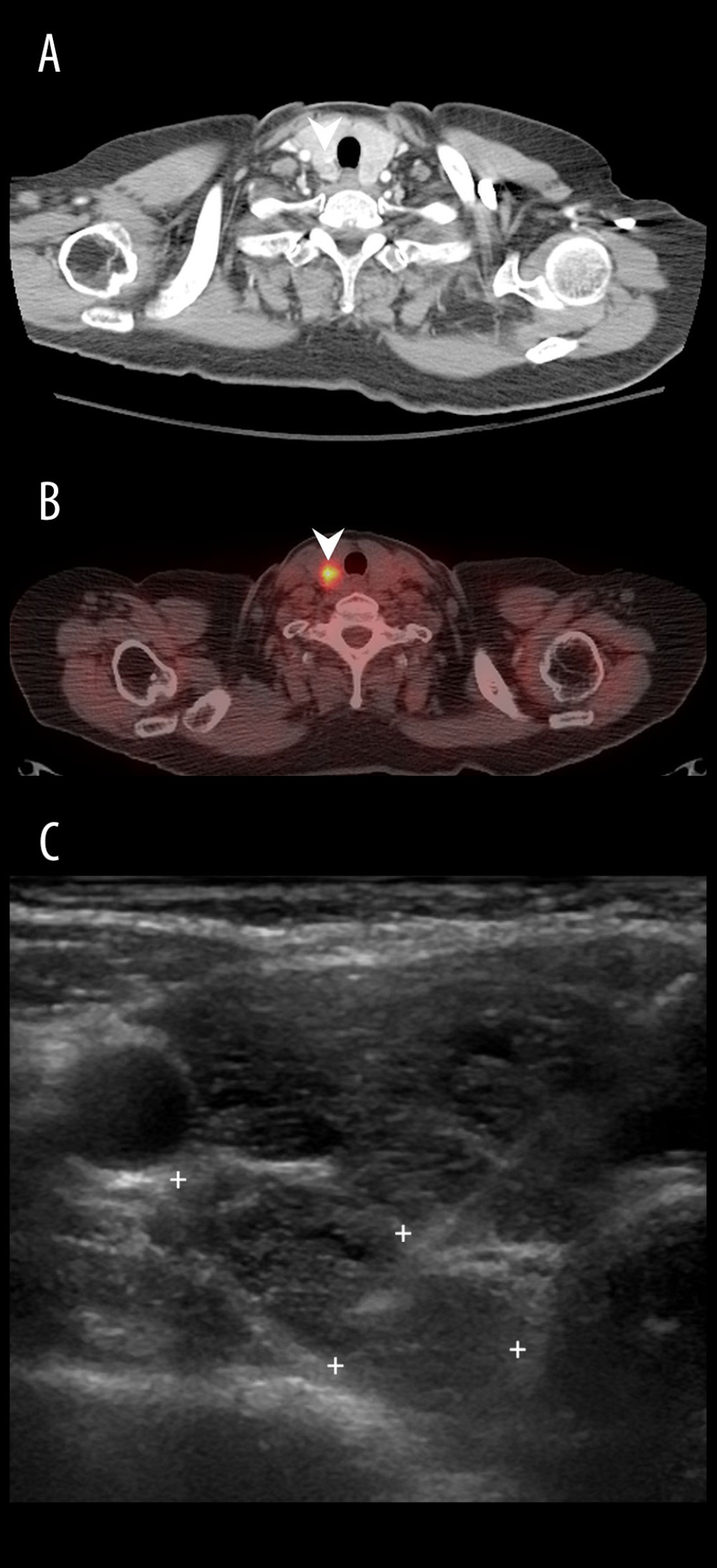 Figure 1. A 61-year-old woman (Patient No. 1) with hepatitis C-related liver cirrhosis and hepatocellular carcinoma was diagnosed with papillary carcinoma (stage I, pT1bN0M0) after total thyroidectomy. (A) Chest CT demonstrated a round isoechoic nodule with contrast-enhanced rim at right lower lobe; (B) 18F-FDG PET/CT showed a hypermetabolic tumor with SUVmax up to 6.8 at right lobe; (C) Transverse view of thyroid echo revealed an ovoid isoechoic tumor at right lower thyroid, then fine needle aspiration disclosed atypical cells.
Figure 1. A 61-year-old woman (Patient No. 1) with hepatitis C-related liver cirrhosis and hepatocellular carcinoma was diagnosed with papillary carcinoma (stage I, pT1bN0M0) after total thyroidectomy. (A) Chest CT demonstrated a round isoechoic nodule with contrast-enhanced rim at right lower lobe; (B) 18F-FDG PET/CT showed a hypermetabolic tumor with SUVmax up to 6.8 at right lobe; (C) Transverse view of thyroid echo revealed an ovoid isoechoic tumor at right lower thyroid, then fine needle aspiration disclosed atypical cells.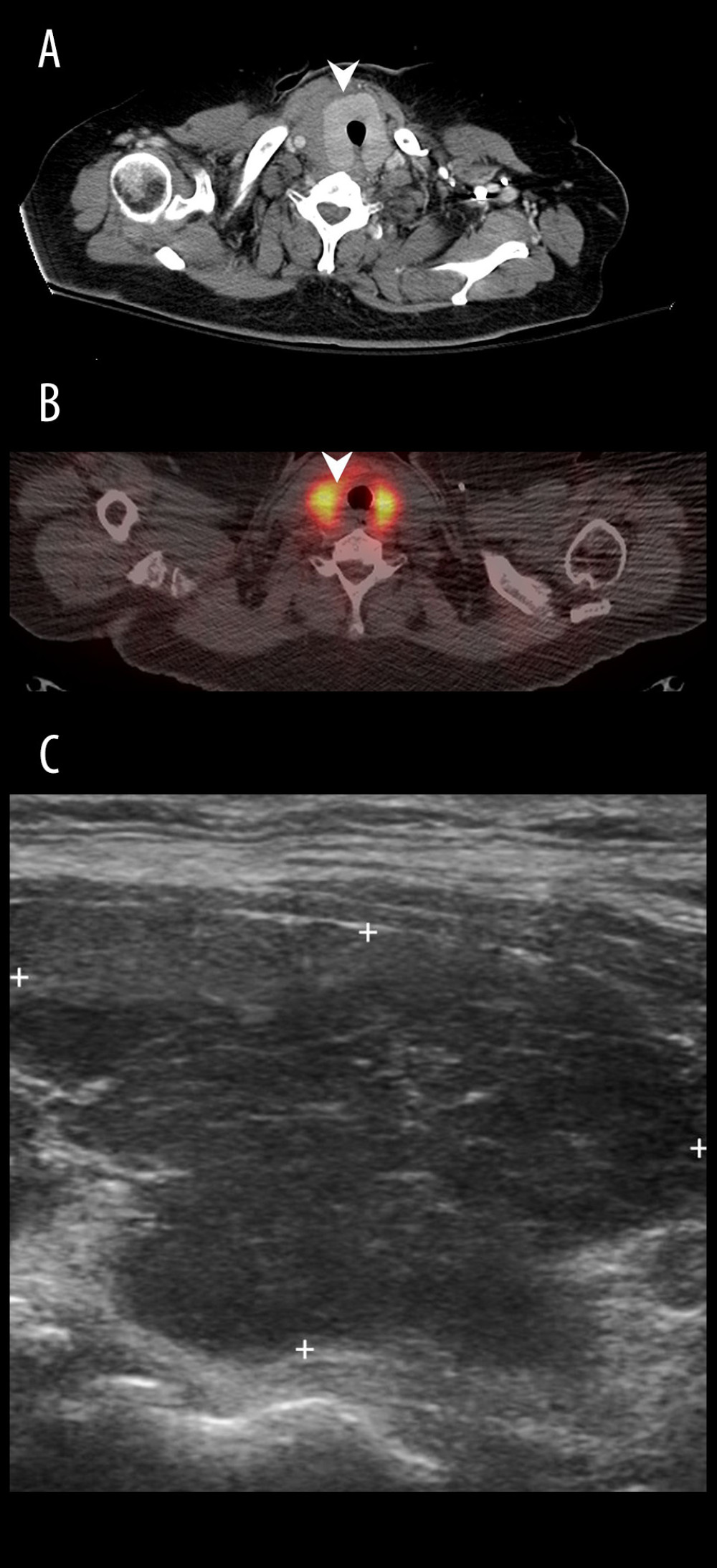 Figure 2. A 60-year-old woman with hepatitis C-related liver cirrhosis. (A) Chest CT showed an enlarged thyroid gland without mass; (B) 18F-FDG PET/CT revealed diffuse uptake over bilateral thyroid with SUVmax up to 12.8; (C) Longitudinal view of thyroid echo disclosed hypoechoic parenchyma, compatible with thyroiditis change.
Figure 2. A 60-year-old woman with hepatitis C-related liver cirrhosis. (A) Chest CT showed an enlarged thyroid gland without mass; (B) 18F-FDG PET/CT revealed diffuse uptake over bilateral thyroid with SUVmax up to 12.8; (C) Longitudinal view of thyroid echo disclosed hypoechoic parenchyma, compatible with thyroiditis change. Tables
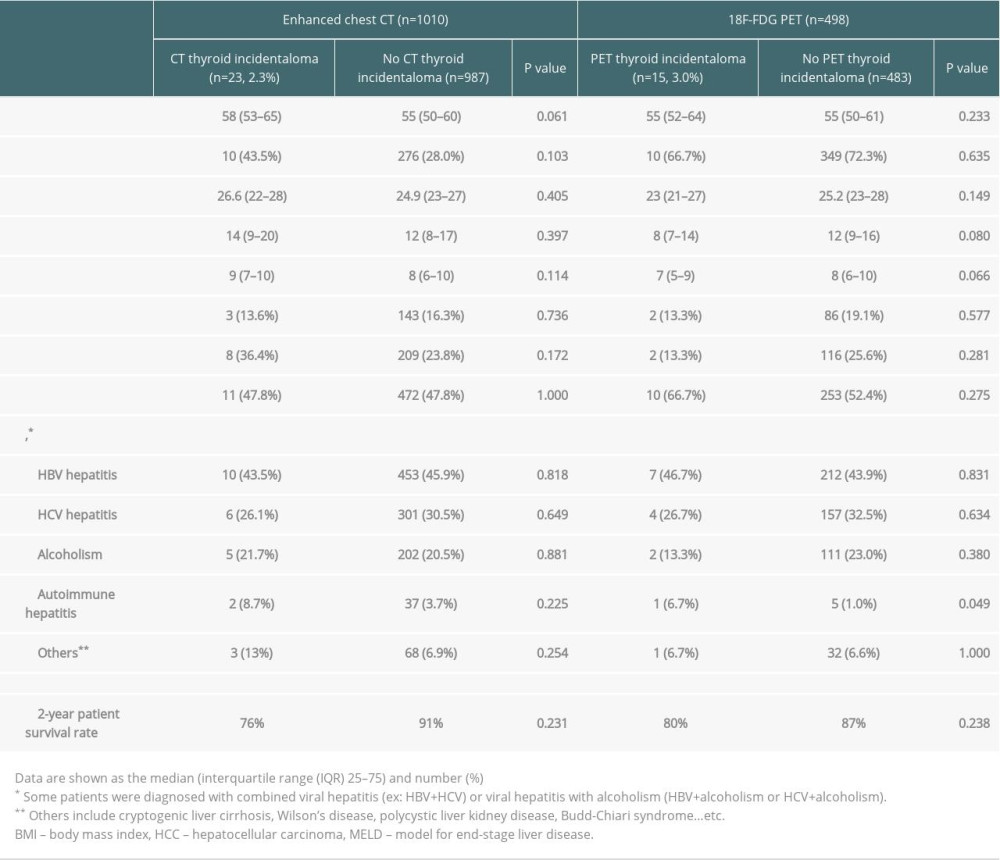 Table 1. Patient characteristics in liver cirrhotic patients waiting for liver transplantation.
Table 1. Patient characteristics in liver cirrhotic patients waiting for liver transplantation.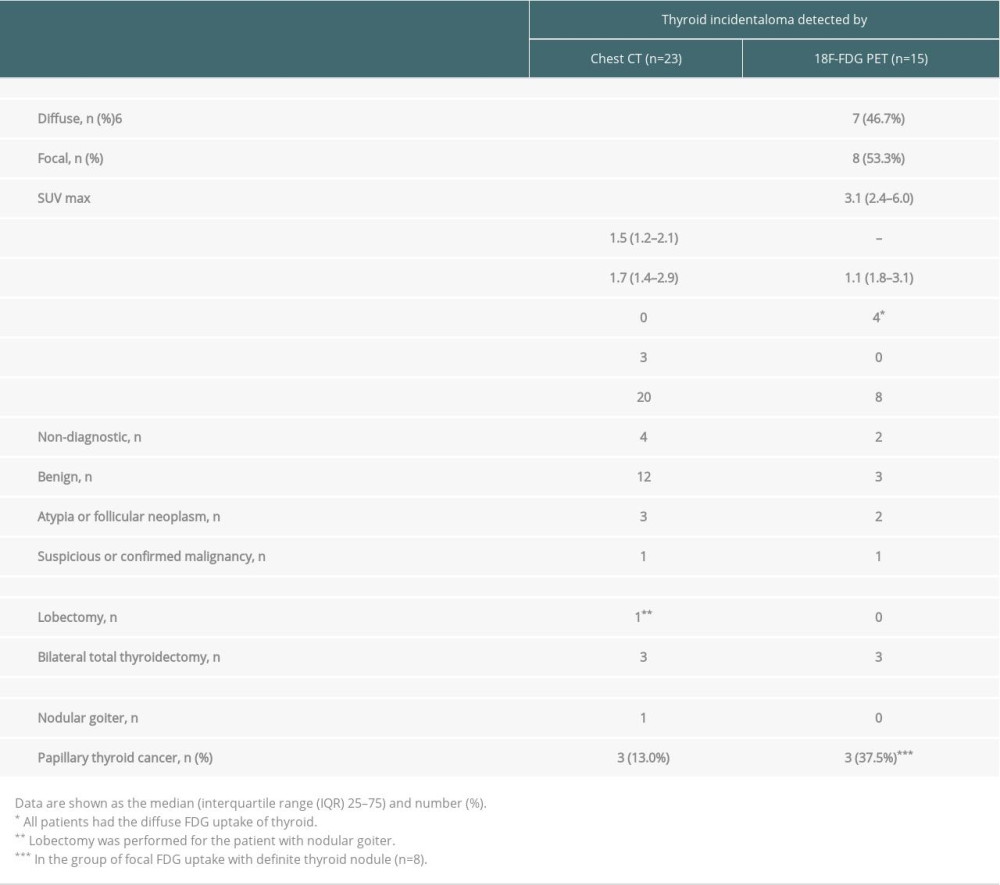 Table 2. Characteristics of the thyroid incidentalomas visualized on CT and PET.
Table 2. Characteristics of the thyroid incidentalomas visualized on CT and PET.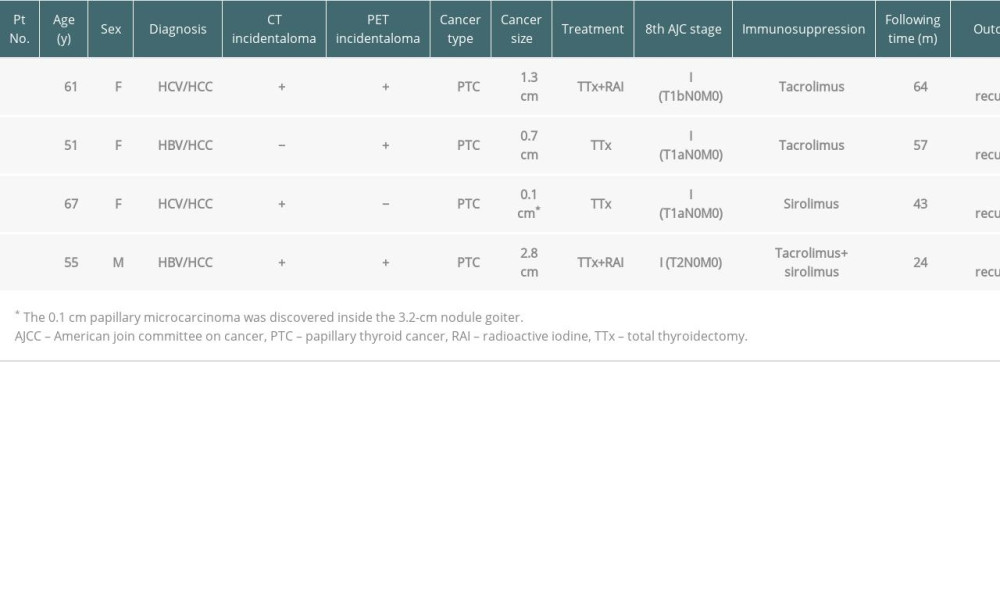 Table 3. Characteristics of LDLT patients diagnosed with incidental thyroid cancer.
Table 3. Characteristics of LDLT patients diagnosed with incidental thyroid cancer.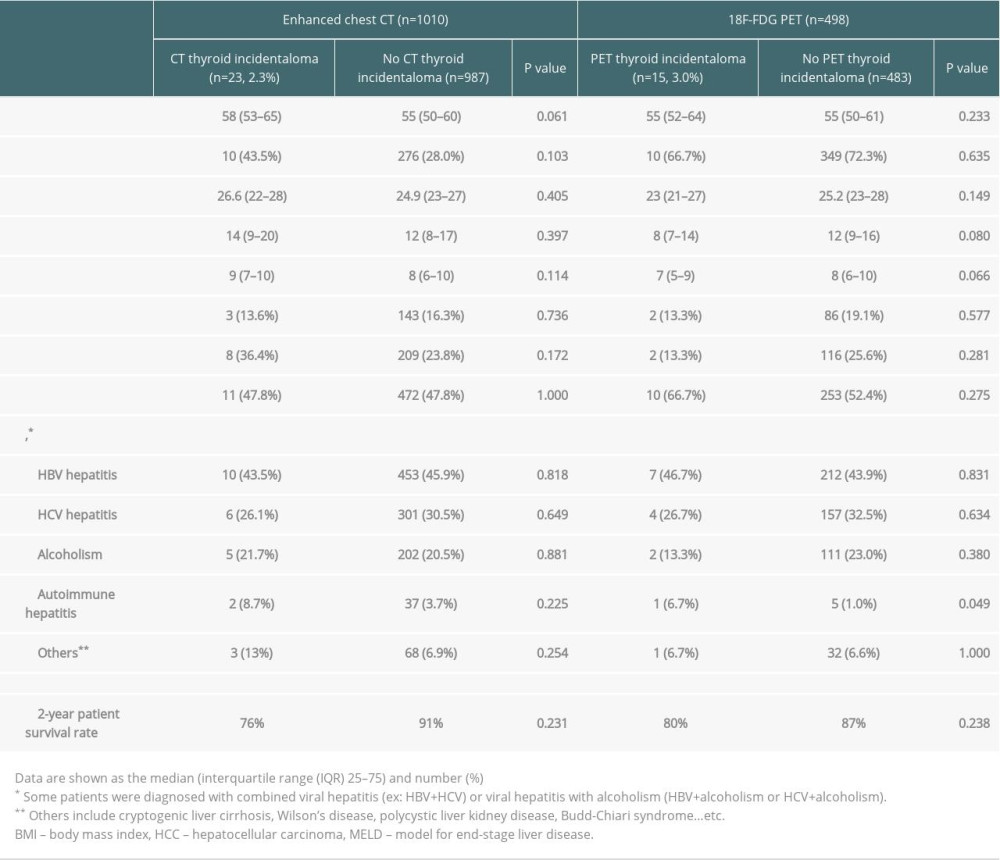 Table 1. Patient characteristics in liver cirrhotic patients waiting for liver transplantation.
Table 1. Patient characteristics in liver cirrhotic patients waiting for liver transplantation.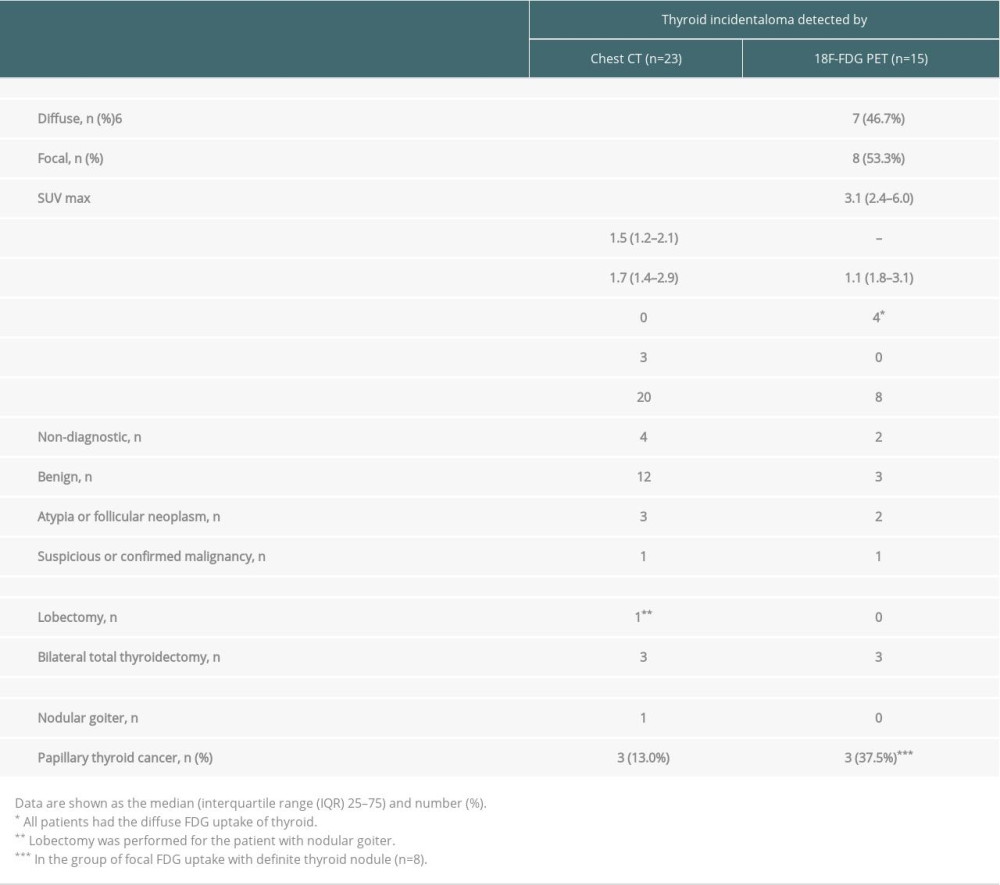 Table 2. Characteristics of the thyroid incidentalomas visualized on CT and PET.
Table 2. Characteristics of the thyroid incidentalomas visualized on CT and PET.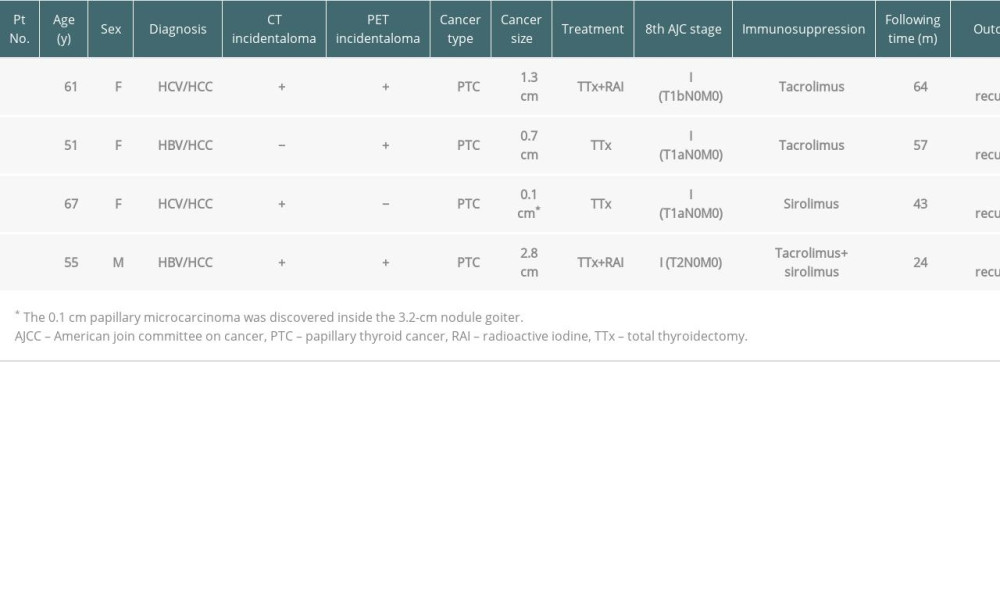 Table 3. Characteristics of LDLT patients diagnosed with incidental thyroid cancer.
Table 3. Characteristics of LDLT patients diagnosed with incidental thyroid cancer. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860








