23 November 2021: Original Paper
The Future Direction of the Organ Donation System After Legislation of the Life-Sustaining Treatment Decision Act
Seung Min Baik1BCEF, Jin Park2BF, Tae Yoon KimDOI: 10.12659/AOT.934345
Ann Transplant 2021; 26:e934345
Abstract
BACKGROUND: The transplant community is seeking ways to encourage organ donation after cardiac arrest to solve the problem of the insufficiency of organs available for the increasing number of people awaiting transplantation. This study aimed to determine whether the life-sustaining treatment (LST) decision system, implemented in Korea on February 4, 2018, can address the shortage of organ donations.
MATERIAL AND METHODS: We retrospectively analyzed the medical records of the 442 patients who had filled out forms for the LST decision at Ewha Womans University Mokdong Hospital from April 2018 to December 2019, and classified the eligibility of organ and tissue donation according to the Korean Organ Donation Agency criteria.
RESULTS: We included 442 patients in this study. Among them, 238 (53.8%) were men, and 204 (46.2%) were women. The average age of the patients was 71.8 years (the youngest and oldest were aged 23 years and 103 years, respectively). Of these, 110 patients (24.9%) decided on their own to discontinue LST, whereas 332 (75.1%) decided to discontinue with their family’s consent. This study demonstrated that 50% of patients who were not brain-dead and discontinued LST were eligible for organ donation. However, the patients and caregivers were not aware of this option because the current law does not allow the discussion of such donations.
CONCLUSIONS: A discussion regarding donation after circulatory death is recommended to solve the problem of insufficient organ donation.
Keywords: Brain Death, Death, Tissue and Organ Procurement, Transplants, Withholding Treatment, Female, Humans, Male, Organ Transplantation, Republic of Korea, Tissue Donors
Background
The number of deaths due to the discontinuation of life-sustaining treatments (LSTs) is gradually increasing worldwide [1–4]. In South Korea, the “Act on Hospice and Palliative Care and Decisions on Life-sustaining Treatment for Patients at the End of Life” was enacted in February 2016, and based on this law, the LST decision system has been implemented since February 4, 2018 [5]. This is a system that allows end-stage patients – those who do not have the possibility of recuperation, did not recover despite treatment, and are on the verge of death with rapidly worsening symptoms or in the process of dying – to independently make decisions regarding continuation of LST, such as cardiopulmonary resuscitation, extracorporeal life support, hemodialysis, chemotherapy, invasive mechanical ventilation, blood transfusion, and vasopressor infusion [1]. If patients are unable to decide on their own dignity of death, South Korea allows all the family members to reach a consensual agreement.
This study aimed to reduce the pain and burden that may be inflicted on dying patients and their families because of meaningless and unnecessary treatment and procedure and to enable the patient to die with dignity. Another purpose was to enable healthy people as well as patients diagnosed with curable or incurable diseases to carefully think and prepare for death [6].
Donation after brain death (DBD) is steadily increasing worldwide. However, the organs available for donation are insufficient for the increasing number of people awaiting transplantation. In the United States, there were 74 078 people awaiting transplantation in 2000, which increased to 113 759 in 2018. Despite this, there were only 11 934 patients eligible to receive an organ transplant in 2000 and 17 554 in 2018 [7]. In South Korea, the number of people waiting for transplantation (excluding tissue transplantation) increased from 2840 in 2000 to 30 544 in 2018, whereas the number of DBD cases increased from 52 in 2000 to 449 in 2018, which was insufficient for the total number of people waiting for transplantation [8]. The domestic transplantation science community is making various efforts to promote organ transplantation surgery, and recently, devising multiple ways to implement donation after circulatory death (DCD).
DCD is the retrieval of organs after the donor’s death for transplantation and confirmed using circulatory criteria, wherein the criteria for brain death are not met [9]. Organ transplantation is being carried out in some countries based on the DCD system [10]. At the beginning of its implementation, unlike organ donation by DBD, organ donation by DCD was associated with poor outcomes after transplantation because it involves organ acquisition in a physical state in which organ perfusion is significantly reduced. However, studies in many countries have reported results similar to those of organ transplantation by DBD [11–17]. Organ transplantation by DCD initially focused on kidney transplantation, but successful results have been recently reported in the liver, lung, and pancreas, which are vulnerable to warm ischemic damage [18–22].
Therefore, this restrospective single-center cohort study aimed to analyze the current status of LST in South Korea and predict whether this can be the basis for DCD legalization. Ultimately, we have provided materials that can contribute to the revitalization of organ donation.
Material and Methods
The medical records of the 442 patients who had filled out forms of the life-sustaining treatment (LST) decisions hoping to terminate their LST at Ewha Womans University Mokdong Hospital from April 2018 to December 2019 were retrospectively analyzed. Demographic characteristics, such as age and sex, of the patients who answered the Physician Orders for Life-Sustaining Treatment (POLST) forms were investigated, and past medical history and diagnosis that made the decision to discontinue LST were confirmed. In terms of disease, the patients were classified into patients with malignant tumor or brain lesions who were judged to be brain-dead, patients with brain lesions who were not brain-dead, and patients with neither brain lesions nor malignant tumors. We investigated the possibility of organ donation, regardless of brain death, on the basis of the patient’s medical history. Organ and tissue donations were classified according to the Korean Organ Donation Agency (KODA).
In addition, we investigated cases of active discontinuation of LST, including withdrawal of vasopressor or inotropics, invasive mechanical ventilator, continuous renal replacement therapy (CRRT), and extracorporeal membrane oxygenation (ECMO), after the LST discontinuation system was implemented.
All numeric variables, such as age, time until death after LST withdrawal (minutes) are expressed as “mean ± standard deviation.” Categorical variables, such as sex, LST decision type, admitted department, diagnosis, death after implementation of LST, LST withdrawal type, and organ donation status of patients who agreed to discontinue LST were analyzed by descriptive statistics. Statistical analysis was performed by using IBM SPSS version 26.0 (SPSS Inc., Chicago, IL, USA). The figure was created by all authors using CorelDRAW 2020 (Corel Corporation, Ottawa, Canada).
Results
The 442 patients included in this study consisted of 238 men (53.8%) and 204 women (46.2%). The average age of the patients was 71.8 years (range: 23–103 years), and those in their 80s accounted for the majority, with 138 people (31.2%). In 110 cases (24.9%), the patients themselves had filled out the POLST form after consulting with the medical staff, and in 332 cases (75.1%) it was a consensual decision made with the family to discontinue LST (Table 1).
Of these patients, 286 patients (64.7%) died; the mean period from the decision to discontinue LST to death was 7.4±13.9 days (minimum 0 days, maximum 144 days). Thirty-three patients died after extubation, vasopressor was withdrawn in 14 patients (3.8%), CRRT was withdrawn in 4 patients (1.4%), and there were no patients with ECMO withdrawal. Patients with mechanical ventilator withdrawal and extubation died within an average of 120 min (2–1218 min), those with vasopressor withdrawal died within an average of 492 min (10–4080 min), and those with CRRT withdrawal died within an average of 232 min (62–420 min) (Table 2).
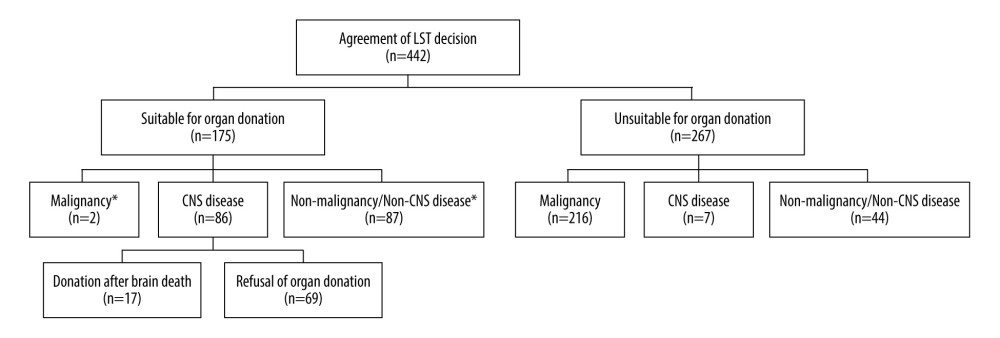
Among those who considered the termination of LST, patients diagnosed with malignant tumors accounted for the majority, with 218 people (49.3%); 93 patients (21%) were diagnosed with central nervous system (CNS) diseases, such as stroke and traumatic and non-traumatic cerebral hemorrhage; and 131 patients (29.6%) had neither malignant tumors nor CNS diseases. The majority of the patients (103, 23.1%) were treated in the Department of Hemato-Oncology, followed by the Department of Pulmonology (74, 16.7%) and the Department of Neurosurgery (56, 12.6%) (Table 1, Figure 1).
Of the 442 patients who agreed to discontinue LST, 175 patients (39.5%) met the organ donor criteria, and 73 (16.5%) were eligible for tissue donation. Of the 175 patients who were eligible for organ donation, 86 had brain lesions, 17 underwent a brain death assessment procedure, and 16 were not assessed. One patient died during the brain death management stage before organ donation. Seventeen patients accounted for 3.8% of all patients who wished to discontinue LST, and only 9.7% of patients were eligible for donation (Figure 1).
Discussion
Unlike DBD, DCD is subject to warm ischemic injury. In general, for DCD, organs are harvested within 5 min after removing the vasopressor, endotracheal tube, and mechanical ventilator and identifying asystole. In other words, the longer the time to reach the asystole state, the longer time the mean arterial pressure was maintained below 65 mmHg, and organ perfusion was decreased. Prolonged exposure to ischemic injury may result in a poor prognosis for transplanted organs or, in the worst case, organ donation and transplantation may become impossible. While the procedure and process of DCD are also important, it is also of paramount importance that the target patient’s risk for mortality within minutes after terminating the treatment is measured. Organs should also be harvested promptly after confirmation of death and, if this is difficult, circulatory recovery through ECMO should be able to maintain organ perfusion until organ procurement [23,24]. To satisfy these conditions in DCD, organ donation after the discontinuation of LST may be the answer.
Patients who depend on LST, such as vasopressors or inotropics, mechanical ventilators, CRRT, and ECMO, become asystolic within minutes or hours after discontinuation of LST. In this study, patients with mechanical ventilator withdrawal and extubation died within an average of 120 min, patients with vasopressor withdrawal died within an average of 492 min, and patients with CRRT withdrawal died within an average of 492 min (Table 2). Therefore, for patients who simultaneously express the intention to discontinue LST and donate organs, a good prognosis of the transplanted organ can be expected if the withdrawal of such LSTs can be coordinated with the timing of organ procurement immediately before transplantation. The time to death after treatment withdrawal depends on the patient’s condition. Therefore, it is appropriate to establish the optimal DCD protocol by conducting large-scale surveys similar to the survey content of this study.
DCD has already been activated globally, and efforts are being made to partially solve the problem of insufficient donor organs [10]. When it comes to DCD, there are still significant differences among countries for various reasons. According to a survey of 28 European countries in 2018, there were 1785 cases of DCD among 11 325 deceased organ donors. This accounted for 15.76% of all deceased organ donors. In 2018, The Netherlands had 164 (58.3%) cases of DCD among 281 deceased organ donors. Interestingly, there were no living organ donors in The Netherlands in 2018. In contrast, 18 countries in Latin America had zero cases of DCD out of 5756 deceased organ donors during the same period [25]. As shown above, the cause of these differences in the number of cases of DCD by country may be the difference in medical technology as well as the lack of agreement on DCD worldwide. There will much debate and it will be a difficult process, but with effort a global consensus may be reached.
Currently, only DBD is deemed acceptable in South Korea, and DCD is subject to various restrictions in practice. However, DBD alone cannot meet the demands of the many patients in need of transplantation. With the LST decision system in place, social discussions and consensus are required before progressing to DCD.
If DCD were allowed in South Korea, as shown in the above results, discussions on organ donation would have occurred in 59 more cases over the past 2 years (Figure 1). Furthermore, as discontinuation of LST is not limited to patients with cancer, it is expected that the establishment of an organ donation system after cardiac arrest will be of great help in promoting transplantation with the legislation of the Life-Sustaining Treatment Decision Act.
For the LST decision system to be properly established, which has finally been implemented after years of discussion, sufficient promotion and explanation should be made to the patients and their caregivers. In addition, if the step to confirm the counselor’s intention to donate organs is added to the process of LST counseling, which is the chance to earnestly consider and accept one’s own death, it will induce a change in perceptions about transplantation and organ donation and promote donation. At Ewha Womans University Mokdong Hospital, especially when the caregivers of brain-dead patients want to stop the LST, the physician in charge explains the donation of organs and tissues. Then, a KODA coordinator who can clearly explain the option and procedure for organ donation would actively advise them to consider it.
Although several candidates for organ donation have been identified, it is controversial whether the LST decision act will lead to organ donation. Therefore, it is necessary to determine the intention to donate organs of those who agreed to LST. As the next step for future study, we will confirm the intention to donate organs by surveying those who directly visited the life-sustaining medical consultation center regarding their decision on LST (and obtain a written statement revealing their decision). Furthermore, this system should be used not only to end life, but also to lead to more organ donations along with institutional development, thus saving more lives.
Conclusions
After years of discussion, the LST decision act was implemented, but the legalization of DCD is still in the discussion stage. However, organ donation is insufficient relative to the increase in the number of people awaiting organ transplantation. Our study suggests that the implementation of LST and the legalization of DCD may solve the insufficient organ donation situation. In countries where DCD has not yet been legalized, such as South Korea, our study will be invaluable as data to demonstrate the need for DCD legalization.
References
1. Sprung CL, Cohen SL, Sjokvist P, End-of-life practices in European intensive care units: the Ethicus Study: JAMA, 2003; 290; 790-97
2. Lesieur O, Leloup M, Gonzalez F, Mamzer MFEPILAT study group, Withholding or withdrawal of treatment under French rules: A study performed in 43 intensive care units: Ann Intensive Care, 2015; 5; 56
3. Angus DC, Barnato AE, Linde-Zwirble WT, Use of intensive care at the end of life in the United States: An epidemiologic study: Crit Care Med, 2004; 32; 638-43
4. Hickman SE, Keevern E, Hammes BJ, Use of the physician orders for life-sustaining treatment program in the clinical setting: A systematic review of the literature: J Am Geriatr Soc, 2015; 63; 341-50
5. National Agency for Management of Life-Sustaining Support Available from: https://www.lst.go.kr/decn/establish.do
6. Lee SI, Hong KS, Park J, Lee YJ, Decision-making regarding withdrawal of life-sustaining treatment and the role of intensivists in the Intensive Care Unit: A single-center study: Acute Crit Care, 2020; 35; 179-88
7. : U.S. Government Information on Organ Donation Transplantation Available from: https://www.organdonor.gov/statistics-stories/statistics/data.html
8. : Korean Network for Organ Sharing (KONOS) Available from: https://www.konos.go.kr/konosis/index.jsp
9. Evrard PBelgian Working Group on DCD National Protocol, Belgian modified classification of Maastricht for donors after circulatory death: Transplant Proc, 2014; 46; 3138-42
10. National Health Service Blood and Transplant Available from: https://www.odt.nhs.uk/deceased-donation/best-practice-guidance/donation-after-circulatory-death/
11. Weber M, Dindo D, Demartines N, Kidney transplantation from donors without a heartbeat: N Engl J Med, 2002; 347; 248-55
12. Thomas I, Caborn S, Manara AR, Experiences in the development of non-heart beating organ donation scheme in a regional neurosciences intensive care unit: Br J Anaesth, 2008; 100; 820-26
13. Summers DM, Johnson RJ, Allen J, Analysis of factors that affect outcome after transplantation of kidneys donated after cardiac death in the UK: A cohort study: Lancet, 2010; 376; 1303-11
14. Akoh JA, Denton MD, Bradshaw SB, Early results of a controlled non-heart-beating kidney donor programme: Nephrol Dial Transplant, 2009; 24; 1992-96
15. Inci I, Donors after cardiocirculatory death and lung transplantation: J Thorac Dis, 2017; 9; 2660-69
16. Summers DM, Watson CJ, Pettigrew GJ, Kidney donation after circulatory death (DCD): state of the art: Kidney Int, 2015; 88; 241-49
17. Tang JX, Na N, Li JJ, Outcomes of controlled donation after cardiac death compared with donation after brain death in liver transplantation: A systematic review and meta-analysis: Transplant Proc, 2018; 50; 33-41
18. White SA, Prasad KR, Liver transplantation from non-heart beating donors: BMJ, 2006; 332; 376-77
19. Tariciotti L, Rocha C, Perera MT, Is it time to extend liver acceptance criteria for controlled donors after cardiac death?: Transplantation, 2011; 92; 1140-46
20. Blok JJ, Detry O, Putter H, Longterm results of liver transplantation from donation after circulatory death: Liver Transpl, 2016; 22; 1107-14
21. Cypel M, Levvey B, Van Raemdonck D, International society for heart and lung transplantation donation after circulatory death registry report: J Heart Lung Transplant, 2015; 34; 1278-82
22. Muthusamy AS, Mumford L, Hudson A, Pancreas transplantation from donors after circulatory death from the United Kingdom: Am J Transplant, 2012; 12; 2150-56
23. Manara AR, Murphy PG, O’Callaghan G, Donation after circulatory death: Br J Anaesth, 2012; 108(Suppl 1); i108-21
24. Halazun KJ, Al-Mukhtar A, Aldouri A, Warm ischemia in transplantation: Search for a consensus definition: Transplant Proc, 2007; 39; 1329-31
25. : Newsletter Transplant International figures on donation and transplantation, 2019 Available from: http://www.transplant-observatory.org/download/newsletter-transplant-2019/e934345-6
Tables
 Table 1. Demographics and disease characteristics of patients who agreed to discontinue life-sustaining treatment.
Table 1. Demographics and disease characteristics of patients who agreed to discontinue life-sustaining treatment.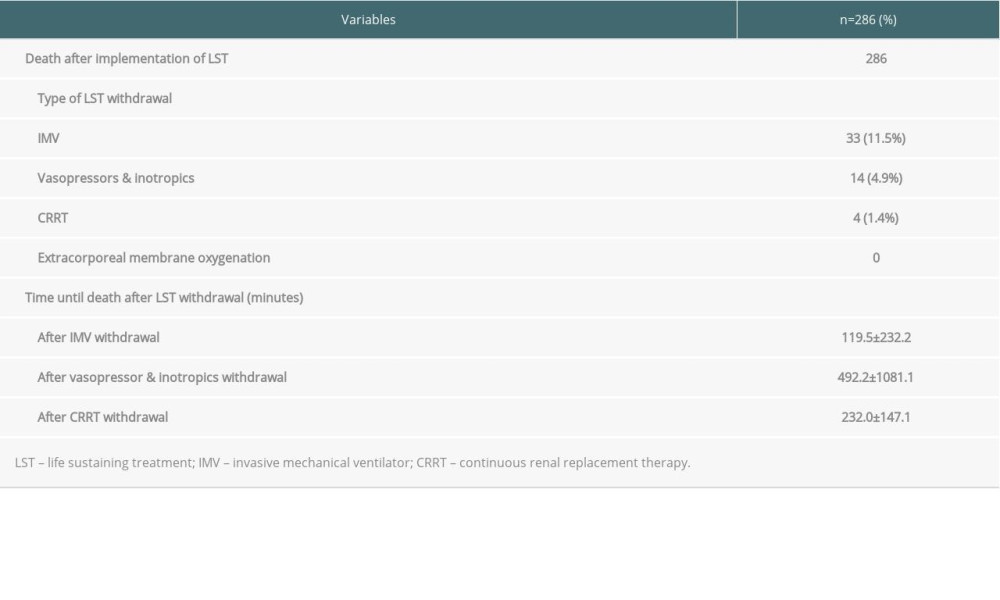 Table 2. Death after implementation of life-sustaining treatment decision.
Table 2. Death after implementation of life-sustaining treatment decision. Table 1. Demographics and disease characteristics of patients who agreed to discontinue life-sustaining treatment.
Table 1. Demographics and disease characteristics of patients who agreed to discontinue life-sustaining treatment. Table 2. Death after implementation of life-sustaining treatment decision.
Table 2. Death after implementation of life-sustaining treatment decision. In Press
15 Mar 2024 : Review article
Approaches and Challenges in the Current Management of Cytomegalovirus in Transplant Recipients: Highlighti...Ann Transplant In Press; DOI: 10.12659/AOT.941185
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860